3690
Quantitative pelvic organ mobility assessment in supine and upright position for assessment of pelvic organ prolapse1Magnetic Detection & Imaging, TechMed Centre, University of Twente, Enschede, Netherlands, 2Laboratoire de mécanique multiphysique multiéchelle, Université de Lille, CNRS, Centrale Lille, Lille, France, 3Multi-Modality Medical Imaging, TechMed Centre, University of Twente, Enschede, Netherlands
Synopsis
Quantitative pelvic organ mobility assessment provides fundamental insight into pelvic organ prolapse (POP). However, this is currently only performed in supine position. In this case study the assessment is performed both in supine and upright position using a tiltable MRI scanner. The displacement of the cervix during contraction is larger in upright than in supine position. During straining the displacement in supine position is 15-20 mm whereas in upright position hardly any displacement occurs. This may indicate that, in upright position, the cervix already reaches its maximum extent at rest. Upright mobility assessment seems to give supplementary information in POP.
Introduction
Pelvic organ prolapse (POP) is a disabling condition and has a prevalence of surgery of almost 20% up to the age of 851. Furthermore, reported anatomical recurrence rates, defined as POP quantification (POP-Q) stage ≥ 2, are up to 40%2. Knowledge about pelvic organ mobility may provide more insight in the effect of surgery on POP, which might enlarge the understanding of the high recurrence rate after POP surgery.MRI is a useful modality for evaluation of pelvic organ mobility, since it can render three-dimensional imaging of the bladder, uterus and rectum simultaneously. Generally, assessment of the extent of POP is based on measuring distances between pelvic organs and the pubococcygeal line (PCL). Organ mobility is defined as the difference between these distances at rest and during contraction/straining. However, this method is observer dependent. Therefore quantitative assessment of the total pelvic organ may provide more objective information about the pelvic organ mobility.
Previous research using quantitative assessment in order to evaluate POP treatment was performed with patients in supine position3. However, since the extent of POP in upright position is significantly larger4, the aims of this research are to perform quantitative assessment of pelvic organ mobility in patients with POP in upright position, and to compare this to the quantitative assessment in supine position.
Methods
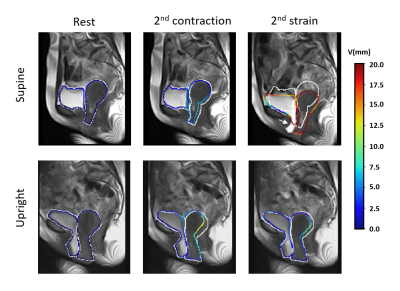
We present a case study of a single patient with POP. Quantitative assessment was performed on the data of an MR scan in supine and upright position (0.25T G-Scan Brio; Esaote S.p.A., Genoa, Italy). A 2D balanced steady-state free precession (bSSFP) sequence was acquired with the following parameters: TE/TR: 3.5/7 ms, reconstructed resolution: 1.5 × 1.5 mm2, slice thickness: 15 mm, FOV: 400 × 400 mm2, flipangle: 70°, acquisition matrix: 160 × 160, total scan time: ≈2s). During acquisition the patient was instructed to contract twice and subsequently strain twice.Image analysis followed the protocol as previously described5. To help results interpretation and measurement validation the contour of pelvic organs are segmented in the initial image. Thereafter, the mobility of organs between the reference image and the deformed image have been quantified using an image registration method and Elastix open-source IR software6. This method consists of calculating the displacement field by comparing initial image (at rest) and subsequent images of the dynamic sequence, based on the flow optic conservation assumption3,5. The displacement field is calculated on the entire image and is extracted on the boundary of organs to analyze and compare their mobility. Finally, the results were visually validated by checking if the contour of the calculated displacement aligned with the observed contour of the MR image.
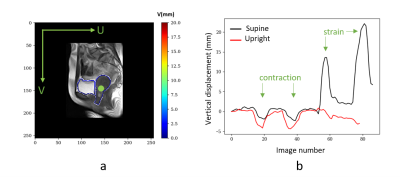
The transformation of each voxel can be described by a vector containing both horizontal (u) and vertical (v) displacement. Because pelvic organ mobility was analyzed in a patient with POP, most displacement was expected in vertical direction. Until now, only the displacement of the cervix was analyzed. This was performed by analyzing the displacement of one point within the cervix contour (Figure 1a) in all images acquired over time with respect to the initial image.
Results
The results of segmentation and displacement analysis are depicted in Figure 2. As shown in Figure 2b, in supine position the vertical displacements of the cervix during contraction and straining are clearly visible (2-3 mm). The displacements during straining are larger than during contraction (15-20 mm), which can also be seen in Figure 1. Furthermore, there is a large difference between the amplitude of vertical displacement of the first and second strain. In upright position the vertical displacement during contraction is larger than in supine position (4-5 mm). There is no clearly identifiable displacement visible during straining, which may indicate that in this patient the cervix already reached its maximum extent at rest.Discussion
This case study shows that the vertical displacement of the cervix during contraction is larger in upright position than in supine position. Displacement during straining is larger in supine position, but varies over each strain, which was already described in literature7.Overall the displaced contour visually matches well with the observed organ. However, extreme mobility of bladder is difficult to capture. Next to that, the quantitative assessment method inherently cannot deal with in and out of plane movement of pelvic organs, as can be seen in Figure 1. 3D imaging can solve this problem, but since this acquisition takes more time than a woman is capable of contraction or straining, this can only be performed at rest. This means that not the difference between rest and strain, but the difference between supine and upright position will be assessed. To translate supine to upright in smaller steps, we can acquire data at different angles of patient position.
The current dataset was acquired without vaginal or rectal contrast. We hypothesize that, especially the insertion of vaginal contrast, has a limited patient burden, but will improve contrast and thereby deformation analyses.
Conclusion
This case study shows that it is feasible to quantitatively determine movement of pelvic organs during contraction and straining in upright and supine position. This is valuable information for assessment of pelvic functionality and makes way for 3D analysis and clinical relevance.Acknowledgements
No acknowledgement found.References
1. De Boer TA, Slieker-Ten Hove MCP, et al., The prevalence and factors associated with previous surgery for pelvic organ prolapse and/or urinary incontinence in a cross-sectional study in the Netherlands. Eur J Obstet Gynecol Reprod Biol. 2011;158(2):343-349.
2. Miedel A, Tegerstedt G, Mörlin B, Hammarström M. A 5-year prospective follow-up study of vaginal surgery for pelvic organ prolapse. Int Urogynecol J. 2008;19(12):1593-1601.
3. van IJsselmuiden MN, Lecomte-Grosbras P, Witz JF, et al., Dynamic magnetic resonance imaging to quantify pelvic organ mobility after treatment for uterine descent: differences between surgical procedures. Int Urogynecol J. 2020.
4. Grob ATM, olde Heuvel J, Futterer JJ, et al. Underestimation of pelvic organ prolapse in the supine straining position, based on magnetic resonance imaging findings. Int Urogynecol J. 2019;30(11):1939-1944.
5. Lecomte-Grosbras P, Witz JF, Brieu M, et al., Quantification of Pelvic Mobility on Dynamic Magnetic Resonance Images: Using Mechanical Insight to Help Diagnose Pelvic Pathologies. Strain. 2015;51(4):301-310.
6. Klein S, Staring M, Pluim JPW. Evaluation of Optimization Methods for Nonrigid Medical Image Registration Using Mutual Information and B-Splines. IEEE Trans IMAGE Process. 2007;16(12).
7. Tumbarello JA, Hsu Y, Lewicky-Gaupp C, et al., Do repetitive Valsalva maneuvers change maximum prolapse on dynamic MRI? Int Urogynecol J. 2010;21(10):1247-1251.
Figures