3689
A preliminary exploration using imaging methods to predict the possibility of the recurrence of serous ovarian cancer undergoing total resection1Radiology, Anhui Provincial Cancer Hospital, Hefei, China, 2Anhui Provincial Cancer Hospital, Hefei, China
Synopsis
The purpose of our research was to define the possibility of the use of imaging methods to analyze and predict the recent recurrence of ovarian serous carcinoma, with the ultimate hope of helping clinicians to plan more suitable treatments. In our study, in CT and MRI examinations before surgery, peritoneal implantation metastasis and Ki67 PI are suggestive of the possibility of the recurrence of serous ovarian carcinoma in the near future, but other imaging indexes show no obvious value for indicating the possibility of recurrence.
INTRODUCTION
The purpose of our research was to explore the value of preoperative CT and MRI examinations and clinical indicators in the prediction of the recurrence of ovarian serous carcinoma in patients who underwent satisfactory staging surgery.METHODS
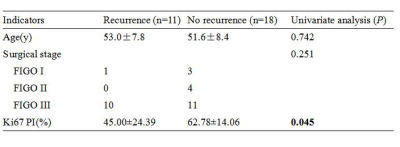
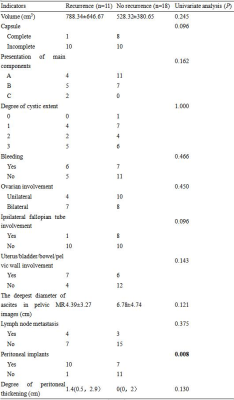
There were 78 patients with histologically proven ovarian serous carcinoma. According to the strict inclusion and exclusion criteria, we retained a total of 29 patients (recurrence group: 11 patients, no recurrence group: 18 patients) for the study. We analyzed the clinical characteristics and CT and MRI features of the two groups. We measured the apparent diffusion coefficient (ADC) value in the tumor solid region and compared the results of the two groups. Univariate analysis was used in the statistical methods of this study.RESULTS
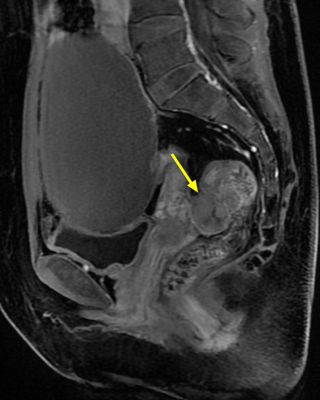
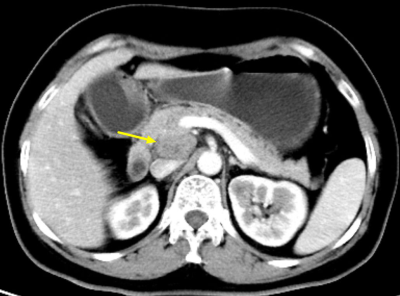
For the Ki67 proliferation index (Ki67 PI) and peritoneal implantation metastasis in CT or MRI images of masses, the difference between the two cohorts was statistically significant (P < 0.05). The rate of peritoneal metastasis in the recurrence cohort (10/11, 91%) was higher than that in the no recurrence cohort (7/18, 39%). The differences in the other preoperative imaging characteristics of ovarian serous cancer, including the volume; capsule of the mass; main components; ADC value; cystic change; bleeding; degree of enhancement of the mainly solid region in 3 periods; and range of tumor involvement in the ovary, fallopian tube, uterus, bladder, bowel, and pelvic wall, were not statistically significant. In addition, the differences in clinical indicators (i.e., age, surgical stage) between the two cohorts were not statistically significant.DISCUSSION
Some past studies have suggested that surgical stage, lymph node metastasis, peritoneal implantation, and abdominal water volume played important roles in the prognosis of ovarian carcinoma.1-4 In our study, except for peritoneal implantation, all the other imaging indicators showed no statistical significance. The reasons are analyzed in detail below. First, as for surgical stage, there were more stage III patients in our study (21/29, 72.4%), while there were fewer stage I and II patients, which may cause a bias in the results. Second, regarding lymph node metastasis, our study described imaging results to assess lymph node metastasis, and previous studies have focused on the results of operations for lymph node metastasis to predict prognosis. These results may not exactly match, as conventional imaging of lymph node metastasis alone may not be able to assess small lymph node metastasis and distinguish it from lymph node reactive hyperplasia. Third, regarding abdominal water quantity, our study measured the deepest diameter perpendicular to the horizontal axis of the pelvic cavity to represent abdominal water quantity, but the results showed no statistical significance, possibly because the pelvic fluid depth could not completely reflect the total amount of fluid in the entire abdomen or pelvis, and some ascites were scattered in the middle and upper levels of the abdominal cavity. Fourth, regarding peritoneal implantation metastasis, our study suggests that preoperative imaging methods were used to assess the peritoneal metastasis in the recurrence group (10/11, 91%) and the no recurrence group (7/18, 39%), with statistical difference judged mainly based on the following signs: multiple peritoneal nodules, irregular peritoneal thickening or thickening similar to a “pie”, and a dirt-like change in the greater omentum. In addition, our study further analyzed the degree of peritoneal thickening, but the results showed no statistical significance. This may imply that no matter how great the degree of peritoneal thickening, the patient’s prognosis was affected as long as there was an implanted metastasis on CT or MRI. In addition to the above indicators, Ki67 PI was statistically significant. The average Ki67 PI of the recurrence cohort was lower than that of the no recurrence cohort, and there was some overlap between the two groups. Previous studies have yielded mixed results for Ki67 PI for prognostic assessment, so the results require further verification with large sample data in the future.In our study, the preoperative imaging characteristics of ovarian serous cancer were retrospectively analyzed in detail, including the volume; capsule of the mass; main components; ADC value; cystic change; bleeding; degree of enhancement of the mainly solid region in 3 periods; and range of tumor involvement in the ovary, fallopian tube, uterus, bladder, bowel, and pelvic wall. These imaging characteristics were rarely observed in the past literature. Although the results were not statistically significant, the negative results are of some important clinical significance, namely, that the preoperative imaging characteristics may reflect only the localized characteristics of the tumor, and reliance on preoperative imaging features to estimate the tumor’s recurrence is very difficult. A combination of imaging methods and clinical indicators to evaluate prognosis, is likely to achieve more meaningful results.CONCLUSION
In CT and MRI examinations before surgery, peritoneal implantation metastasis and Ki67 PI are suggestive of the possibility of the recurrence of serous ovarian carcinoma in the near future, but other imaging indexes showed no obvious value for indicating the possibility of recurrence.Acknowledgements
No acknowledgement found.References
1. Pereira A, Perez-Medina T, Magrina J F, et al. The impact of debulking surgery in patients with node-positive epithelial ovarian cancer: Analysis of prognostic factors related to overall survival and progression-free survival after an extended long-term follow-up period. Surg Oncol. 2016; 25(1): 49-59.
2. H.H. Chung, M. Lee, H.S. Kim, et al. Prognostic implication of the metastatic lesion-to -ovarian cancer standardised uptake value ratio in advanced serous epithelial ovarian cancer. Eur Radiol. 2017; 27(11): 4510-4515.
3. GAN Xiaojing, ZHOU Yong, WEN Zhi. Influence of CT Manifestations, Tumor Marker Levels and Pathology on Ovarian Cancer Recurrence. Chinese Journal of Medical Imaging. 2016; 24(2): 133-137.
4. Chen Y, Zhang L, Liu WX, et al. Prognostic significance of preoperative anemia, leukocytosis and thrombocytosis in chinese women with epithelial ovarian cancer. APJCP. 2014; 16(3): 933-939.
Figures