3628
Quantification of strain analysis in coronary chronic total occlusion: A cardiovascular magnetic resonance imaging follow-up study1Department of Radiology, Beijing AnZhen Hospital, Capital Medical University, Beijing, China, 2Department of Cardiology, Beijing AnZhen Hospital, Capital Medical University, Beijing, China, 33Siemens Shenzhen Magnetic Resonance Ltd, Beijing, China, 4Department of Radiology, Beijing Friendship Hospital, Capital Medical University, Beijing, China
Synopsis
This study investigated the benefits of percutaneous coronary intervention (PCI) in patients with chronic total occlusions (CTOs) by using cardiac magnetic resonance imaging (CMR)-feature tracking (CMR-FT).The results showed the infarct size and LVEF did not increase significantly from baseline to 1 year of follow-up.However, global peak strains improved over time, and GCS showed significant treatment effect of CTO-PCI in the entire CMR population,which indicated improvement in left ventricular function.
Purpose
The present study aimed to investigate the benefits of percutaneous coronary intervention (PCI) in patients with chronic total occlusions (CTOs) by using cardiac magnetic resonance imaging (CMR)-feature tracking (CMR-FT).Methods
Fifty-two patients with successful CTO-PCI underwent CMR (3T, MAGNETOM Verio, Siemens Healthineers, Erlangen, Germany) at baseline and 12 months after successful PCI. CMR-FT was applied to cine images to measure left ventricle (LV) global radial, circumferential, and longitudinal peak strains (GRS, GCS, and GLS, respectively), and grayscale thresholds of 5 standard deviations (SDs) were used to quantify late gadolinium enhancement (LGE). We categorized patients with CTOs into the viable and nonviable groups (with the cutoff of segmental infarct extent (SIE) < 50%). Major adverse cardiac events were defined as cardiac death, acute myocardial infarction, and hospitalization for heart failure.Figure 1 shows example of CMR feature tracking (FT) for quantification of myocardial deformation.Results
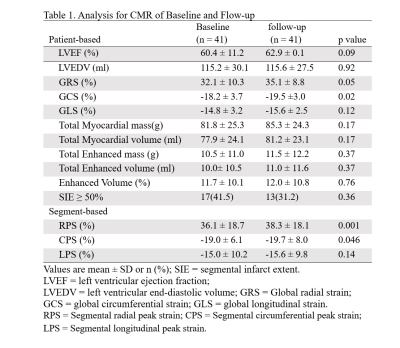
From December 2014 to November 2019, 64 of the 192 patients with CTO underwent baseline and follow-up CMR. Among them, 52 patients underwent PCI successfully. Four patients with acute MI within 3 months before PCI and seven patients with limited MR images were excluded. Over a median follow-up period of 12 months (range: 8–29 months), 41 patients (55.3 ± 10.9 years, 82.9% males) with successful CTO-PCI were included in data analysis. During the follow-up (median,12 months), no patient experienced major adverse events.In the total CMR population, the mean baseline left ventricular ejection fraction (LVEF) was 60.4 ± 11.2%, left ventricular end diastolic volume (LVEDV) was 115.2 ± 30.1 ml, and total enhanced mass (TEM) was 10.5 ± 11.0 g. Furthermore, 73% of patients with CTOs showed no reduction in LVEF (>50%). Left ventricle GRS, GCS, and GLS were 32.1 ± 10.3%, -18.2 ± 3.7%, and -14.8 ± 3.2%, respectively (Table 1). GRS, GCS, and GLS by CMR-FT were strongly correlated with LVEF (r = 0.83, r = 0.83, r = 0.67, respectively, p < 0.05 for all). GRS and GCS were moderately correlated with TEM (r = 0.48, r = 0.49, respectively, p < 0.05 for both). Baseline characteristics of the study population are shown in Tables 1 and 2.
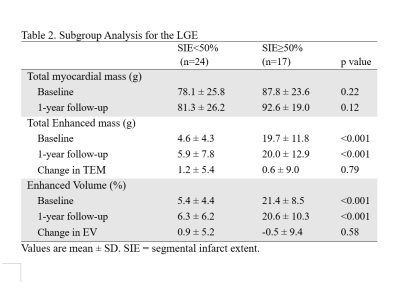
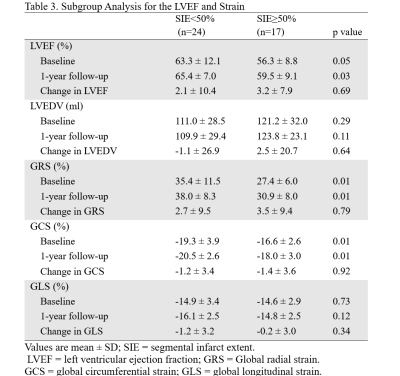
The LVEF of the viable group was higher than that of the nonviable group (63.3 ± 12.1 vs. 56.3 ± 8.8, p = 0.05). The TEM of the nonviable group was significantly higher than that of the viable group (19.7 ± 11.8 g vs. 4.6 ± 4.3 g, p < 0.001) (Table 2). Mean baseline GRS and GCS values of the viable group were significantly higher than those of the nonviable group (35.4 ± 11.5% vs. 27.4 ± 6.0%, -19.3 ± 3.9% vs. -16.6 ± 2.6%, all p < 0.05). However, there were no significant differences between the two groups in mean baseline GLS and LVEDV values (Table 3).
In this study of CTO-PCI, in the entire CMR population and subgroup analysis, the infarct size did not increase significantly from baseline to 1 year of follow-up (p > 0.05 for all). LVEF did not show significant improvement in the 1-year follow-up (60.4 ± 11.2% vs. 62.9 ± 0.1%, p = 0.09) in the entire CMR population. However, global peak strains improved over time, and GCS showed significant treatment effect of CTO-PCI in the entire CMR population (Δ GRS 3.0 ± 9.3%, p = 0.05; Δ GCS -1.3 ± 3.4%, p = 0.02; ΔGLS − 0.8 ± 3.1%, p = 0.12) (Table 1).
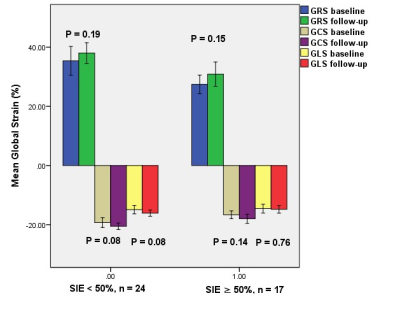
In the subgroup analysis, the mean follow-up GRS and GCS values of the viable group were significantly higher than those of the nonviable group (38.0 ± 8.3% vs. 30.9 ± 8.0%, -20.5 ± 2.6% vs. -18.0 ± 3.0%, all p < 0.05). However, the mean GLS value of the viable group was not significantly higher than that of the nonviable group at follow-up (-16.1 ± 2.5% vs. -14.8 ± 2.5%, p = 0.12) (Figure 2).
Discussion
LVEF reflects the global function of the LV, but it cannot distinguish the regional myocardial strain in different directions, and it cannot reflect the early damaged function of heart disease. CMR-FT technology provides an incremental value for risk stratification in various cardiac diseases.In our present study, the mean GLS at baseline (-14.8%) was lower than -20%, without significant improvement after PCI. Therefore, although LVEF of most CTOs in the present study did not decrease significantly during the 1-year follow-up, GLS decreased and did not improve after successful PCI, which may be considered as a potential risk factor.The independent prognostic value of GCS is controversial. GCS in our study showed treatment effect of CTO-PCI on the recovery of global strain parameters. Kenneth et al showed that circumferential strain has independent prognostic importance in study participants with acute ST-segment elevation myocardial infarction. However, other follow-up studies of acute MI did not support this finding. Thus, more evidence needs to be provided in the future.
Conclusions
In this single center study, GCS showed treatment effect of successful CTO-PCI at 1-year follow-up in our study, which indicated improvement in left ventricular function.Acknowledgements
No acknowledgement found.References
1. Danek BA, Karatasakis A, Tajti P, et al. Incidence, treatment, and outcomes of coronary perforation during chronic total occlusion percutaneous coronary intervention. Am J Cardiol. 2017; 120(8):1285-92. DOI: 10.1016/j.amjcard.2017.07.010
2. Elias J, van Dongen IM, Råmunddal T, et al. Long-term impact of chronic total occlusion recanalisation in patients with ST-elevation myocardial infarction. Heart. 2018; 104(17):1432-8.
3. Henriques JP, Hoebers LP, Råmunddal T, et al. Percutaneous intervention for concurrent chronic total occlusions in patients with STEMI: The Explore Trial. J Am Coll Cardiol. 2016; 68(15):1622-32.
4. Lee SW, Lee PH, Ahn JM, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion. Circulation. 2019 Apr 2;139(14):1674-83. DOI: 10.1161/CIRCULATIONAHA.118.031313
5. Grün S, Schumm J, Greulich S, et al. Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. J Am Coll Cardiol. 2012; 59(18):1604-15. DOI: 10.1016/j.jacc.2012.01.007
6. Claus P, Omar AMS, Pedrizzetti G, et al. Tissue Tracking Technology for Assessing Cardiac Mechanics: Principles, Normal Values, and Clinical Applications. JACC: CARDIOVASCULAR IMAGING. 2015 Dec;8(12):1444-60. doi: 10.1016/j.jcmg.2015.11.001.
7. Andre F, Steen H, Matheis P, et al. Age- and gender-related normal left ventricular deformation assessed by cardiovascular magnetic resonance feature tracking. Journal of Cardiovascular Magnetic Resonance. 2015 Mar 10;17(1):25. doi: 10.1186/s12968-015-0123-3.
8. Vo HQ, Marwick TH, Negishi K. MRI-Derived Myocardial Strain Measures in Normal Subjects. JACC: CARDIOVASCULAR IMAGING. 2018 Feb;11(2 Pt 1):196-205. doi: 10.1016/j.jcmg.2016.12.025. 9. Zhang LJ, Dong W, Li JN, et al. Quantification of Late Gadolinium Enhancement Cardiovascular Magnetic Resonance Imaging in Patients with Coronary Artery Chronic Total Occlusion. Clinical Radiology. 2020 Aug;75(8):643.
10. Bulluck H, Hammond-Haley M, Weinmann S, et al. Myocardial Infarct Size by CMR in Clinical Cardioprotection Studies: Insights From Randomized Controlled Trials. JACC Cardiovasc Imaging. 2017 Mar;10(3):230-40. doi: 10.1016/j.jcmg.2017.01.008.
11. Kowallick JT, Morton G, Lamata P, et al. Inter-study Reproducibility of Left Ventricular Torsion and Torsion Rate Quantification Using MR Myocardial Feature Tracking. Journal of Magnetic Resonance Imaging. 2016 Jan;43(1):128-37. doi: 10.1002/jmri.24979.
12. Taylor RJ, Moody WE, Umar F, Edwards NC, Taylor TJ, Stegemann B, Townend JN, Hor KN, Steeds RP, Mazur W, Leyva F (2015) Myocardial strain measurement with feature-tracking cardiovascular magnetic resonance: normal values. Eur Heart J. doi:10.1093/ehjci/jev006
13. A ndre F, Steen H, Matheis P, Westkott M, Breuninger K, Sander Y, Kammerer R, Galuschky C, Giannitsis E, Korosoglou G, Katus HA, Buss SJ (2015) Age- and gender-related normal left ventricular deformation assessed by cardiovascular magnetic resonance feature tracking. J Cardiovasc Magn Reson 17(1):25. doi:10.1186/s12968-015-0123-3
14. Satriano A, Heydari B, Narous M, et al. Clinical feasibility and validation of 3D principal strain analysis from cine MRI: comparison to 2D strain by MRI and 3D speckle tracking echocardiography. Int J Cardiovasc Imaging 2017 Dec;33(12):1979–92. DOI 10.1007/s10554-017-1199-7.
15. Almutairi HM, Boubertakh R, Miquel ME, et al. Myocardial deformation assessment using cardiovascular magnetic resonance-feature tracking technique. Br J Radiol. 2017 Dec;90(1080):20170072. doi: 10.1259/bjr.20170072.
16. Cho GY, Marwick TH, Kim HS, et al. Global 2-dimensional strain as a new prognosticator in patients with heart failure. J Am Coll Cardiol 2009 Aug 11;54(7):618-24. doi: 10.1016/j.jacc.2009.04.061.
17. Buss SJ, Emami M, Mereles D, et al. Longitudinal left ventricular function for prediction of survival in systemic light-chain amyloidosis: incremental value compared with clinical and biochemical markers. J Am Coll Cardiol 60(12):1067–76. doi:10.1016/j. jacc.2012.04.043
18. Korosoglou G, Gitsioudis G, Voss A, et al. Strainencoded cardiac magnetic resonance during high-dose dobutamine stress testing for the estimation of cardiac outcomes: comparison to clinical parameters and conventional wall motion readings. J Am Coll Cardiol 2011 Sep 6;58(11):1140-9. doi:10.1016/j. jacc.2011.03.063
19. Romano S, Judd RM, Kim RJ, et al. Association of feature-tracking cardiac magnetic resonance imaging left ventricular global longitudinal strain with all-cause mortality in patients with reduced left ventricular ejection fraction. Circulation 2017;135: 2313–5.
20. Romano S, Judd RM, Kim RJ, et al. Feature tracking global longitudinal strain predicts death in a multicenter population of patients with ischemic and nonischemic dilated cardiomyopathy incremental to ejection fraction and late gadolinium enhancement. J Am Coll Cardiol Img 2018;11: 1419–29.
21. Buss SJ, Breuninger K, Lehrke S, et al. Assessment of myocardial deformation with cardiac magnetic resonance strain imaging improves risk stratification in patients with dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 2015;16: 307–15.
22. Romano S, Judd RM, Kim RJ, et al. Feature-tracking global longitudinal strain predicts mortality in patients with preserved ejection fraction. JACC Cardiovasc Imaging. 2020 Apr;13(4):940-947. doi: 10.1016/j.jcmg.2019.10.004.
23. Zhang Z, Ma QZ, Cao LZ, et al. Correlation between left ventricular myocardial strain and left ventricular geometry in healthy adults: a cardiovascular magnetic resonance‑feature tracking study. The International Journal of Cardiovascular Imaging. 2019 Nov;35(11):2057-65. doi: 10.1007/s10554-019-01644-3.
24. Mordi I, Bezerra H, Carrick D, et al. The combined incremental prognostic value of left ventricular ejection fraction, late gadolinium enhancement and global circumferential strain assessed by cardiovascular magnetic resonance. Journal of Cardiovascular Magnetic Resonance 2015, 17(Suppl 1): Q50
25. Mangion K, Carrick D, Carberry J. et al. Circumferential strain predicts major adverse cardiovascular events following acute segment–elevation myocardial infarction. Radiology. 2019 Feb;290(2):329-337. doi: 10.1148/radiol.2018181253.
26. Eitel I, Stiermaier T, Lange T, et al. Cardiac magnetic resonance myocardial feature tracking for optimized prediction of cardiovascular events following myocardial infarction. JACC Cardiovasc Imaging 2018 Feb 9. pii: S1936-878X(17)31176-2 [Epub ahead of print].
27. Gavara J, Rodriguez-Palomares JF, Valente F, et al. Prognostic value of strain by tissue tracking cardiac magnetic resonance after ST-segment elevation myocardial infarction. JACC Cardiovasc Imaging 2017 Dec 8. pii: S1936-878X(17)30985-3 [Epub ahead of print].
28. Yoon YE, Kang SH, Choi HM, et al. Prediction of infarct size and adverse cardiac outcomes by tissue tracking-cardiac magnetic resonance imaging in ST segment elevation myocardial infarction. Eur Radiol 2018;28(8):3454–3463.
29. Buckert D, Kelle S, Buss S, et al. Left ventricular ejection fraction and presence of myocardial necrosis assessed by cardiac magnetic resonance imaging correctly risk stratify patients with stable coronary artery disease: a multi-center all-comers trial. Clin Res Cardiol. 2017; 106(3):219 - 29.
30. Coleman GC, Shaw PW, Balfour PC Jr, et al. Prognostic value of myocardial scarring on CMR in patients with cardiac sarcoidosis. JACC Cardiovasc Imaging. 2017; 10(4):411-420.
31. Schumacher SP, Everaars H, Stuijfzand WJ, et al. Coronary collaterals and myocardial viability in patients with chronic total occlusions. EuroIntervention. 2020 Aug 7;16(6):e453-e461. doi: 10.4244/EIJ-D-19-01006.
32. Li JN, He Y, Dong W, et al. Comparison of cardiac MRI with PET for assessment of myocardial viability in patients with coronary chronic total occlusion. Clinical Radiology. 2019 May;74(5):410.e1-410.e9. doi: 10.1016/j.crad.2019.01.021.
Figures