3466
Assessment of Spinal Cord Diffusivity in Degenerative Cervical Myelopathy after Spinal Fusion Decompression1Radiology, Medical College of Wisconsin, Milwaukee, WI, United States, 2Neurosurgery, Medical College of Wisconsin, Milwaukee, WI, United States
Synopsis
Metal artifacts from commonly-encountered spinal fusion stabilization hardware have historically confounded quantitative MRI (qMRI) research investigations of the injured and damaged spinal cord in human subjects. This report provides preliminary analysis of metal-artifact suppressed multi-spectral diffusion qMRI collected on instrumented degenerative cervical spondylotic myelopathy (CSM) subjects. The results of the study demonstrate group trends of reduced diffusivity in the CSM group at spinal cord levels fused by hardware. This is a unique finding in instrumented CSM subjects that may offer unique insight into the impact of spinal fusion interventions on conventional qMRI measures of the spinal cord.
Introduction
Degenerative cervical spondylotic myelopathy (CSM) of the spinal cord is the most common cause of spinal dysfunction in adults. Quantitative DW MRI has been shown to have significant correlations with clinical presentation and outcomes in CSM1. However, MRI of CSM in post-surgical subjects in the spinal cord at levels fused with stabilization hardware has never been attempted due to the substantial limitations of conventional DWI near metallic devices.This report provides preliminary analysis of metal-artifact suppressed multi-spectral diffusion weighted MRI2 collected at fused levels in instrumented CSM subjects in a range of 3 months to 12 months after surgery (mean 6 months). The quantitative apparent diffusion coefficient (ADC) values derived using automated processing pipeline are compared to an asymptomatic non-instrumented control cohort using an identical imaging protocol and region of interest analysis.
Methods
This preliminary analysis provides results of 9 CSM subjects (age: 56.1+/-9.1 yrs, gender: 7F, 2M ) treated with spinal fusion (time since procedure: 6 +/3 months ) and 13 asymptomatic controls (age: 43.1 +/- 16.8 yrs, gender: 10 F, 3 M ). Subjects provided written consent into a study protocol approved by the Medical College of Wisconsin IRB. CSM subjects underwent a Modified Japanese Orthopaedic Association Scale (mJOA) symptom checklist (cohort score: 14.3 +/- 3.5) indicating moderate neurological dysfunction (max score: 18).Magnetic Resonance Imaging was performed at 3 Tesla on a GE Signa Premier system utilizing the vendor-provided 21 channel head-neck reception array.
All key study sequences utilized multi-spectral imaging metal artifact reduction techniques. Morphological imaging was performed using 1.2mm isotropic T1 and T2 weighted MAVRIC SL acquisitions. Diffusion-weighted imaging was performed using the MAVRIC DWI approach, which leverages PROPELLER DUO spin-echo based diffusion-weighted imaging2. DWI were acquired in the axial plane obliqued perpendicular to the spinal cord at 1.6mm^2 in-plane resolution with 5mm slice thickness and 2 to 3 stations of 2-5 slices seeking to cover C3 to C7 vertebral levels of the cord. Diffusion weighting was achieved with one b=0 image and three diffusion encoded images along each of the Cartesian axis at b = 600 s/mm^2.
Data were analyzed using the Spinal Cord Toolbox (SCT)3. Briefly, the T2w MAVRIC SL image was utilized for deep-learning-based SCT cord segmentation and vertebral labeling. The spinal cord regions of interest were applied to the MAVRIC DWI images for whole-cord ADC quantification. Manual quality assurance was also utilized to inspect and refine each auto-generated cord region of interest using the computed ADC maps as a reference. ADC values were reported for each slice and accumulated across levels and subjects. Non-parametric Mann-Whitney U-tests were used to assess the ADC values across 3 groups: 1) instrumented fused levels in CSM subjects, 2) non-fused levels in CSM subjects, and 3) all levels in control subjects.
Results
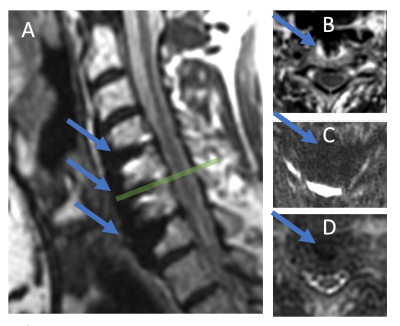
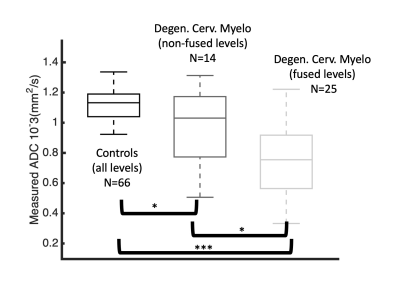
Figure 1 provides a demonstration of the advantages of multi-spectral MAVRIC DW approaches for assessments of the cord at instrumented levels compared to echo planar imaging. A sagittal T2w MAVRIC SL image (A) indicates (arrows) fusion hardware that causes severe distortions in the reduced field of view EPI (FOCUS) DW image (C). The DW MAVRIC image (D) clearly depicts the spinal cord contour even in the presence of the hardware at this level.Figure 2 provides summary values of the MAVRIC DWI distributions from the CSM and healthy subjects. Of note, the instrumentation-fused level measurements showed substantially reduced ADC relative to both control (p < 0.0001) and non-fused levels (p = 0.03). The non-fused levels were reduced relative to the control group, but to a lesser degree (p = 0.04) and with more variability than the fused levels.
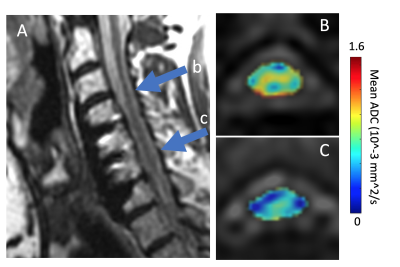
Figure 3 provides exemplary images of the MAVRIC DW ADC measurements on one subject, at levels indicated in the MAVRIC T2w image (A) that are (B) above the level of instrumented fusion and (C) at the level of fusion. The stark differences in the ADC values across the cord in these different levels are readily apparent.
No statistically significant correlations were identified between any of the analysis groups and clinical mJOA scores
Discussion
Though previous studies have identified substantial reductions in diffusivity after post-surgical decompression with fixation in CSM patients4, the results of this preliminary study analysis offer unique insight into increased reductions at fused levels. Previous findings reported by Sato et al4 found reductions in diffusivity after non-instrumented decompression procedures that nominally recovered back to normal levels by 6 months. Given the mean duration of time from fusion surgery in the present cohort (6 +/- 3 months), these new results suggest that a lower baseline of diffusivity may exist in fused levels for a longer time duration.Due to the relatively small sample size and limited range of mJOA impairment across this cohort of CSM subjects (14.3 +/- 3.5), the lack of a significant correlation between ADC and mJOA is not unexpected. Whether these ADC decreases in the post-surgical cord have meaningful insight to the recovery profile or success of decompression remains to be determined. Nonetheless, the considerable improvement in image quality with MAVRIC DWI compared to the more common DWI-EPI opens the door to larger cohorts and further examination of spinal cord integrity.
Acknowledgements
Supported by the Department of Defense Broad Agency Announcement for Extramural Medical Research through award number W81XWH1910273References
1. Rao, Avinash, Hesham Soliman, Mayank Kaushal, Olesya Motovylyak, Aditya Vedantam, Matthew D. Budde, Brian Schmit, Marjorie Wang, and Shekar N. Kurpad. "Diffusion tensor imaging in a large longitudinal series of patients with cervical spondylotic myelopathy correlated with long-term functional outcome." Neurosurgery 83, no. 4 (2018): 753-760.2.
2. Koch, K. M., Bhave, S., Gaddipati, A., Hargreaves, B. A., Gui, D., Peters, R., Kaushik, S., Multispectral diffusion-weighted imaging near metal implants. Magnetic Resonance in Medicine, (2018 )86-A, 1947–7.3.
3. De Leener B, Levy S, Dupont SM, Fonov VS, Stikov N, Louis Collins D, Callot V, Cohen-Adad J. SCT: Spinal Cord Toolbox, an open-source software for processing spinal cord MRI data. Neuroimage 20164.
4. Sato, T., T. Horikoshi, A. Watanabe, M. Uchida, K. Ishigame, T. Araki, and H. Kinouchi. Evaluation of cervical myelopathy using apparent diffusion coefficient measured by diffusion-weighted imaging. American journal of neuroradiology 33, no. 2 (2012): 388-392.
Figures