3465
Spaceflight Associated Neuro-Ocular Syndrome: Quantitative MRI Evaluation of Lower Body Negative Pressure as a Potential Countermeasure1Diagnostic Imaging, UTHSC-Houston, Houston, TX, United States, 2NASA, Houston, TX, United States, 3KBR, Houston, TX, United States, 4Orthopedic Surgery, UCSD, La Jolla, CA, United States
Synopsis
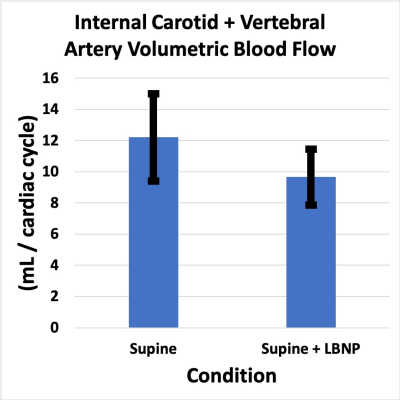
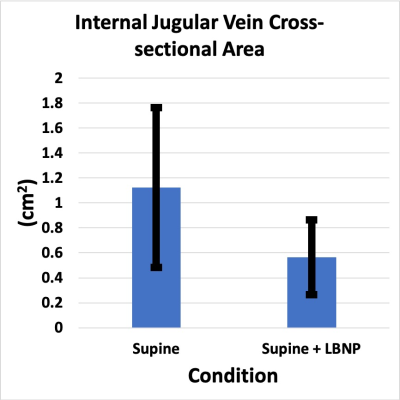
The application of lower body negative pressure in the supine position significantly reduces bulk cerebral arterial flow and cross-sectional area of the internal jugular vein compared to the supine position alone. This is similar to the physiologic response expected with upright compared to supine positioning. Our results suggest that lower body negative pressure applied during spaceflight may help reduce headward fluid shift and venous congestion and mitigate the development of optic disc edema associated with long-duration spaceflight.
PURPOSE
Optic disc edema develops in two-thirds of astronauts exposed to long duration spaceflight (1,2) and is part of a spectrum of findings referred to as spaceflight associated neuro-ocular syndrome (SANS). Chronic headward fluid shift and venous congestion, invariably present in spaceflight due to the absence of a 1G gravitational vector, are hypothesized causes of SANS (3,4). Preliminary results obtained at the Cardiovascular and Vision laboratory at NASA Johnson Space Center suggest that lower body negative pressure (LBNP) is a promising countermeasure to reduce headward fluid shift and venous congestion. At 1G, headward fluid shift and venous congestion are reproduced in the supine or head-down tilt positions. Physiologically the upright position is associated with a decrease in internal jugular vein cross-sectional area and bulk cerebral blood flow compared to the supine position(5). Using quantitative MRI techniques, our goal was to determine if LBNP applied during supine positioning can approximate these same physiological responses associated with upright positioning thereby further supporting LBNP as a potential spaceflight countermeasure of SANS.METHODS
Nine healthy volunteers (5 women, 4 men, mean age = 39 ± 9 years, mean BMI = 26 ± 4 kg/m2) provided written consent to participate in this study. MRI scans were performed on a 3T Magnet using a 16-channel head coil. The following sequences were utilized: A 3D T1-weighted FSPGR sequence for brain volumetric assessment, pseudo-continuous arterial spin labelling to determine cerebral perfusion, pulse-gated phase-contrast sequences to evaluate bulk cerebral arterial, internal jugular venous, and aqueductal CSF flow characteristics. All volunteers were scanned in the supine position without LBNP, and in the supine position with 25 mmHg LBNP, in a randomized order. Total imaging time was approximately 2 hours for each subject. Blood pressure, heart rate and oxygen saturation were monitored during the entire MRI procedure.RESULTS
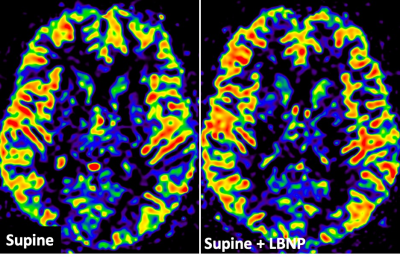
Oxygen saturation during LBNP was 97 ± 2% compared to 98 ± 2% without LBNP (p=.08). Blood pressure during LBNP was 120/71 ± 12/7 mmHg compared to 125/76 ± 15/11 mm Hg without LBNP (p=.12). Heart rate was 71± 2 BPM during LBNP compared to 64 ± 9 BPM without LBNP (11% increase; p=.0002). Cerebral arterial flow during LBNP was 9.6 ± 1.8 mL/s compared to 12.2 ± 2.8 mL/s without LBNP (21% decrease; p=.007). Internal jugular vein cross-sectional area during LBNP was 56 ± 31 mm2 compared to 112 ± 64 mm2 without LBNP (50% decrease; p=.03). Internal jugular vein blood flow during LBNP was 6.5 ± 3.1 mL/s compared to 9.3 ± 3.5 mL/s without LBNP (30% decrease; p=.002). Combined brain + total CSF volume, lateral ventricular volume, arterial resistive index, and aqueductal CSF peak-to peak velocity were unchanged during application of LBNP (p=.09; p=.12). Whole brain white matter and gray matter perfusion during LBNP were 23.4 ± 4.3 mL/100 gm/min and 36.9 ± 8.0 mL/100 gm/min respectively compared to 24.8 ± 5.7 mL/100 gm/min and 38.3 ± 8.4 mL/100 gm/min without LBNP (p=.24; p=.26).CONCLUSION
Short-term application of 25 mmHg LBNP in the supine position causes a significant reduction in cerebral arterial blood flow, internal jugular vein blood flow and internal jugular cross-sectional area with increased heart rate compared to the supine position without LBNP. LBNP also showed no significant impact on white or gray matter cerebral perfusion, arterial vascular resistance, blood oxygenation, blood pressure, combined brain + total CSF and lateral ventricular volumes or CSF hydrodynamics. Therefore the application of LBNP during supine posture shifts physiology towards that expected with the upright posture. This is achieved without detriment to blood oxygenation or cerebral perfusion. Simulation of upright posture physiology with LBNP could potentially help reduce headward fluid shifts and venous congestion within the microgravity environment. Further research is needed to determine if the application of LBNP can prevent SANS associated with long-duration spaceflight.Acknowledgements
Supported by the NASA Human Research Program 80NSSC19K1668References
1. Macias BR, Patel NB, Gibson CR, Samuels BC, Laurie SS, Otto C, Ferguson CR, Lee SMC, Ploutz-Snyder R, Kramer LA, Mader TH, Brunstetter T, Stenger MB. Association of Long-Duration Spaceflight With Anterior and Posterior Ocular Structure Changes in Astronauts and Their Recovery. JAMA Ophthalmol 2020;138(5):553-559. doi: 10.1001/jamaophthalmol.2020.0673
2. Kramer LA, Sargsyan AE, Hasan KM, Polk JD, Hamilton DR. Orbital and intracranial effects of microgravity: findings at 3-T MR imaging. Radiology 2012;263(3):819-827. doi: 10.1148/radiol.12111986
3. Kramer LA, Hasan KM, Stenger MB, Sargsyan A, Laurie SS, Otto C, Ploutz-Snyder RJ, Marshall-Goebel K, Riascos RF, Macias BR. Intracranial Effects of Microgravity: A Prospective Longitudinal MRI Study. Radiology 2020:191413. doi: 10.1148/radiol.2020191413
4. Marshall-Goebel K, Laurie SS, Alferova IV, Arbeille P, Aunon-Chancellor SM, Ebert DJ, Lee SMC, Macias BR, Martin DS, Pattarini JM, Ploutz-Snyder R, Ribeiro LC, Tarver WJ, Dulchavsky SA, Hargens AR, Stenger MB. Assessment of Jugular Venous Blood Flow Stasis and Thrombosis During Spaceflight. JAMA Netw Open 2019;2(11):e1915011. doi: 10.1001/jamanetworkopen.2019.15011
5. Alperin N, Hushek SG, Lee SH, Sivaramakrishnan A, Lichtor T. MRI study of cerebral blood flow and CSF flow dynamics in an upright posture: the effect of posture on the intracranial compliance and pressure. Acta Neurochir Suppl 2005;95:177-181
Figures