3223
Identification of COPD Lesions Using 3D Ultrashort Echo-Time Imaging with Ventilation Map and Ventilation Flow Map1Department of Biomedical Engineering, Sungkyunkwan University, Suwon, Korea, Republic of, 2Biomedical Institute for Convergence at SKKU, Sungkyunkwan University, Suwon, Korea, Republic of, 3Department of Radiology and Center for Imaging Science, Samsung Medical Center, Seoul, Korea, Republic of, 4Department of Intelligent Precision Healthcare Convergence, Sungkyunkwan University, Suwon, Korea, Republic of
Synopsis
Chronical Obstructive Pulmonary Disease (COPD) is an obstructive lung disease and mainly consists of emphysema and chronic bronchitis. Recent works proposed for the quantitative evaluation of emphysema severity based on the signal intensity of UTE lung images. Through this study, MRI, as well as CT, can represent the defect region for the ventilation defect region, and furthermore, the degree of the lesion and the ventilation function of the lungs can be evaluated such as ventilation map, ventilation flow map and histogram. The potential of methods was validated by ventilation map, ventilation flow map and ventilation histogram in emphysema patient.
Introduction
Lung MRI has several challenging issues such as short T2*, low proton density, respiratory motion, and large magnetic susceptibility difference between lung tissue and air, and these challenges can be overcome to some extent with ultrashort echo time (UTE) imaging techniques1. UTE Lung MRI can be used for providing structural information, as well as functional information such as ventilation map.Chronical Obstructive Pulmonary Disease (COPD) is an obstructive lung disease and mainly consists of emphysema and chronic bronchitis. In emphysema, alveolar membranes break down and ventilation function decreases. On the other hand, chronic bronchitis causes inflammation of airway lumen and excess mucus. One of the COPD studies is PREFUL2 (Phase Resolved Functional MRI), a method that uses Fourier decomposed and reconstructed images such as perfusion maps and ventilation maps. In addition, another interesting method was recently proposed for the quantitative evaluation of emphysema severity based on the signal intensity of UTE lung images3, considering that destroyed alveolar membrane in emphysema can lead to the reduction of tissue proton density from a MRI standpoint.
In this study, we investigated how COPD lesions including emphysema appear in ventilation map and ventilation flow map from a functional standpoint.
Methods
Ventilation map: Ventilation map is typically obtained by calculating the voxel-wise signal difference between end-inspiration and end-expiration after image registration4, and defect regions with ventilatory dysfunction appear dark in ventilation map showing less signal difference: $$Ventilation=(S(\text{end expiration})-S(\text{end inspiration}))/(S(\text{end expiration}))\times100$$ .Ventilation flow map: To evaluate air flow in ventilation, we employed the concept of the fractional ventilation (FV) flow2, which is defined as ,$$Ventilation flow=(\triangle FV)/(\triangle t), \text{ where } FV=(S(\text{end expiration})-S(\text{t}))/(S(\text{end expiration}))\times100.$$. The ventilation flow map is then determined by calculating the voxel-wise difference between the maximum and minimum ventilation flow.
Imaging: This study was approved by the Institutional Review Board of Samsung medical center and performed in full accordance with guidelines. One patient (85 years, male) with severe emphysema underwent lung MRI and dual-energy CT. Lung MRI was performed at 3T (Skyra, Siemens) using a 34-channel chest coil for reception and body coil for transmission. For lung imaging, volume-selective 3D UTE sequence (VS-UTE) was used with fat suppression5,6,7. VS-UTE effectively suppresses the signals coming from the outside of FOV and considerably reduces streak artifacts which often appear in conventional 3D UTE-MRI. Scan parameters were TR/TE = 2.8/0.2 ms, FOV = 360 mm, FA = 5°, number of radial views = 150k, matrix size = 440×440×440, isotropic resolution = 0.82 mm. For ventilation map, images were reconstructed again to a lower resolution (=2 mm) in order to further increase the signal-to-noise ratio (SNR). A self-navigation method developed by our group was used to trace the respiratory motion8. CT images were acquired in a dual-energy CT system (105 mAs at 140 kV; 248 mAs at 80 kV) with a matrix size of 512×512.
Data Processing and Analysis: Images were reconstructed with a home-built MATLAB program using FFT with gridding. A retrospective respiratory gating was performed to obtain the end-expiration and end-inspiration images. The number of radial views at each respiratory phase was set to be same as 18k. To obtain the ventilation map, image registration and volume segmentation were performed using ANTs and home-built segmentation tool using a convolutional neural network (CNN), respectively.
Results and Discussion
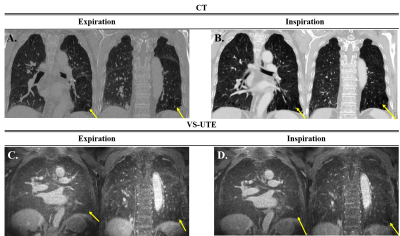
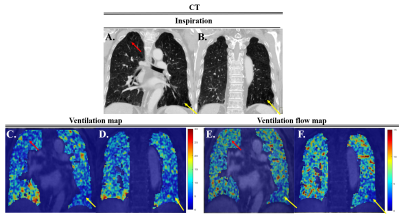
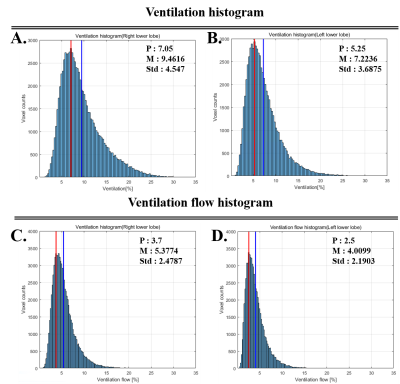
Figure 1 show the anatomical images of lung CT and UTE-MRI acquired at end-expiration (A,C) and end-inspiration (B,D). As indicate by yellow arrows, the emphysema lesions seen in the CT images were also identified in the UTE images in the left lower lobes. Figure 2 shows the ventilation maps (C,D) and ventilation-flow maps (E,F) obtained from UTE images. The same emphysema lesions in the left lower lobes could also be identified as low signal intensities on the ventilation maps (yellow arrows). It is interesting to note that the right upper lobe shows low signal intensity on the ventilation map, whereas the same region appears normal on the ventilation flow map (red arrows). According to this observation, small airway disease can be suspected in the right upper lobe. Figure 3 show the ventilation (A,B) and ventilation-flow (C,D) histograms in the right (A C) and left (B,D) lower lobes. As expected from Fig.2, overall ventilation (or peak or mean position) looked higher in the right lower lobe (A) than the left lower lobe (B) because of the severe emphysema in the left lower lobe, and overall ventilation flow also looked higher in the right lobe (C) than the left lobe (D).Conclusion
Here, we demonstrated that ventilation and ventilation-flow maps as well as UTE-MRI can also identify emphysema lesions. In addition, we found that additional information for other COPD lesions, e.g., small airway disease, could also be obtained when there exists a difference between ventilation and ventilation flow. A further study is warranted for a large cohort of patients with obstructive and restrictive pulmonary diseases. We expect that functional information such as ventilation and ventilation flow maps including the histogram can be used to diagnose COPD phenotypes and disease progression, together with structural information of UTE-MRI.Acknowledgements
This study was supported by National Research Foundation of Korea NRF-2020R1A2B5B02002676 and NRF-2018-Global Ph.D. Fellowship Program.References
1. Bergin CJ, Pauly JM, Macovski A. Lung parenchyma : projection reconstruction MR imaging. Radiology. 1991;179(3):777-781.
2. Andreas Voskrebenzev et al. Feasibility of quantitative regional ventilation and perfusion mapping with phase-resolved functional lung (PREFUL) MRI in healthy volunteers and COPD, CTEPH, and CF patients. Magn Reson Med . 2018 Apr;79(4):2306-2314.
3. Benlala et al. Automated Volumetric Quantification of Emphysema Severity by Using Ultrashort Echo Time MRI: Validation in Participants with Chronic Obstructive Pulmonary Disease
4. Zapke M et al. Magnetic resonance lung function--a breakthrough for lung imaging and functional assessment? A phantom study and clinical trial. Respir Res. 2006 Aug 6; 7:106. Radiology. 2019 Jul;292(1):216-225.
5. Jinil Park and Jang-Yeon Park. Reducing Streak Artifacts in 3D Radial Imaging Using Volume-Selective Signal Acquisition. Proc. Intl. Soc. Mag. Reson. Med. 28 (2020)
6. Jang-Yeon Park et al. Short echo-time 3D radial gradient-echo MRI using concurrent dephasing and excitation. Magn. Reson. Med. 2012; 67 (2): 428–436.
7. Jinil Park et al. A radial sampling strategy for uniform k-space coverage with retrospective respiratory gating in 3D ultrashort-echo-time lung imaging. NMR Biomed. 2016; 29: 576–587.
8. Jinil Park et al. A Robust Self-navigation for Respiratory Gating in 3D Radial Ultrashort Echo-time Lung MRI using Concurrent Dephasing and Excitation. Journal of the Korean Physical Society, Vol. 73, No. 1, July 2018, pp. 138∼144.
Figures