3208
Pulmonary functional imaging for lung adenocarcinoma: combined MRI assessment based on IVIM-DWI and OE-UTE-MRI1Department of Radiology, Fourth Hospital of Hebei Medical University, Shijiazhuang, China, 2United Imaging Healthcare, Shanghai, China
Synopsis
Despite the introduction of new treatment options in recent years, the survival rates of patients with lung adenocarcinoma (LUAD) remain unsatisfactory. In order to care for patients effectively, clear insight into the processes of ventilation and perfusion of LUAD is required. In this work, Intravoxel incoherent motion diffusion weighted imaging (IVIM-DWI) was used to monitor the blood flow while oxygen-enhanced MRI (OE-MRI) was used to measure the ventilation. Our results showed that the combined measurement of OE-MRI and IVIM-DWI may serve as a promising method for the noninvasive assessment of lung function and classification of LUAD subtype.
Introduction
Lung cancer remains the leading cause of global cancer incidence and mortality, and 70% patients were only diagnosed in advanced stage 1. Lung adenocarcinoma (LUAD) is the most common histological subtype accounting for approximately 40% of all lung cancers 2.LUAD can disrupt the delicate tissue architecture and compromise gas exchange across alveoli, which severely impact the quality of life and long-term survival of the patients. Ventilation, blood flow and their inter-relationship are the major determinants of gas exchange in the lungs 3. Thus, in order to care for patients effectively, clear insight into the processes of ventilation and perfusion of LUAD is required. Intravoxel incoherent motion diffusion weighted imaging (IVIM-DWI) has demonstrated the ability to separate reflection of tissue diffusivity and microcapillary perfusion in lung cancer 4, while oxygen-enhanced MRI (OE-MRI) has demonstrated the ability to measure pulmonary ventilation globally and regionally 5.
The goal of current study was to introduce a noninvasive and reproducible MRI method for in vivo functional assessment of the whole lung and specific lesions.
Materials and Methods
PatientsSixteen patients with pathologically confirmed LUAD were included in this study. According to the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) classification 6, five major growth patterns were defined by two experienced pathologists: lepidic, acinar, papillary, micropapillary and solid. The predominant pattern was designated for each tumor. Spirometry was performed according to American Thoracic Society guidelines 7 and the gas transfer was measured by the diffusing capacity for carbon monoxide per litre alveolar volume and adjusted for hemoglobin (DLCOc/VA).
MRI examination
MRI examinations were performed on a 3.0 Tesla system (uMR 780, United Imaging Healthcare, Shanghai, China) with a commercial phased-array 12-channel torso coil. The OE-MRI was based on a respiratory-gated 3D radial ultra-short echo time (UTE) sequence (TR/TE = 2.2/0.08 ms, slice thickness = 2 mm, FOV = 350×350 mm2, matrix = 480×480, FA = 8°). The parameters used for diffusion weighted single-shot spin-echo based echo-planar imaging were TR/TE = 4000/1.4 ms, slice thickness = 5 mm, FOV = 380×380 mm2, Matrix = 256×256, FA = 90°, b-values = 0, 10, 20, 30, 50, 80, 100, 200, 400, and 800 s/mm2.
OE-MRI analysis
3D-UTE was performed twice for each subject. The first was acquired during free-breathing with 21% oxygen (normoxic), while the second was acquired with 100% oxygen (hyperoxic). Two minutes of 100% oxygen inhalation was performed before the second UTE measurement to avoid the transit effect.The normoxic and hyperoxic images were coregistered by rigid transform and B-spline symmetric normalization (SyN) transform 8 with a mutual information metric using Advanced Normalization Tools (http://stnava.github.io/ANTs). The hyperoxic images were segmented to produce a binary lung mask and a binary tumor mask using 3D slicer 9. Then, the percent signal enhancement (PSE) map for the whole lung and each tumor were calculated by the expression
$$PSE = (S100% - S21%) / S21%$$
where S21% and S100% are signals acquired during room air and 100% oxygen inhalation, respectively.
IVIM analysis
For each tumor, IVIM analysis was performed by an in-house prototype software developed by Matlab R2018b. In the bi-exponential IVIM model, signal behavior follows:
$$Sb/S0 = (1-f) x exp (-b x D) + f x exp (-b x D*)$$
where f is the fractional perfusion related to microcirculation, D is the true diffusion as reflected by pure molecular diffusion, and D* is the pseudo-diffusion coefficient related to perfusion.
Statistics
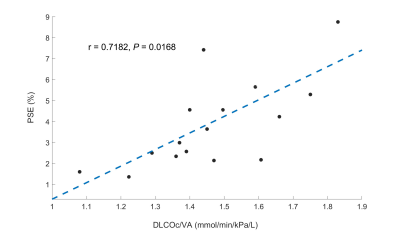
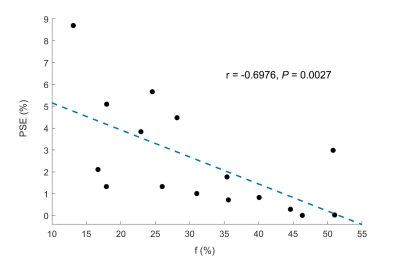
Spearman’s test was used to assess the relationship between (a) whole lung mean PSE and DLCOc/VA; (b) lesion mean PSE and IVIM-derived parameters.
Results
The most frequent LUAD subtype in this study was acinar predominant (50%), followed by lepidic predominant (37.5%). Besides, one papillary predominant and one micropapillary predominant were included (6.25%, respectively). Table 1 summarizes the mean PSE and IVIM-derived parameters for these four subtypes. According to the statistical analysis, whole lung mean PSE was significantly correlated with DLCOc/VA (r = 0.7182, P = 0.0168) (Figure 1). lesion mean PSE was negatively correlated with f (r = -0.6976, P = 0.0027) (Figure 2).Discussion & Conclusion
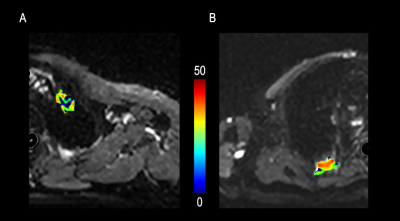
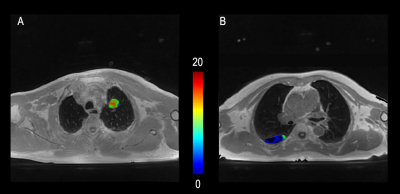
In this work, the global lung PSE measured with OE-UTE-MRI showed strong correlation with DLCOc/VA, which supports the hypothesis that gas transfer can be visualized in MRI by using OE-UTE-MRI. Besides, OE-UTE-MRI is further superior to conventional PFTs in regional analysis. Our result showed significant negative relationship between lesion mean PSE and f. The increase of vascularity may involve the higher consumption of gas and thus results in a lower ventilation. This regional result suggested that MRI can add fundamental insights into pathophysiologic mechanism, by tailoring to specific lung regions and disease phenotypes. In line with prior research, micropapillary predominant adenocarcinoma was the subtype with the lowest disease-specific survival rate, while the lepidic predominant adenocarcinoma predicted favorable prognosis 10. As shown in Figure 3 and 4, compared to lepidic predominant adenocarcinoma, micropapillary predominant adenocarcinoma showed higher f and lower mean PSE.This study suggested that the combined measurement of OE-UTE-MRI and IVIM-DWI may serve as a promising method for the noninvasive assessment of lung function and classification of LUAD subtype. Further research with larger sample size is needed to support this preliminary study.
Acknowledgements
No acknowledgement found.References
1. Travis WD. Pathology of lung cancer. Clinics in chest medicine. 2011;32(4):669-692.
2. Bhimji S, Wallen J. Cancer, Lung, Adenocarcinoma. 2018.
3. Prisk GK. Ventilation, Blood Flow, and Their Inter‐Relationships. Cotes’ Lung Function. 2020:259-299.
4. Wang L-l, Lin J, Liu K, et al. Intravoxel incoherent motion diffusion-weighted MR imaging in differentiation of lung cancer from obstructive lung consolidation: comparison and correlation with pharmacokinetic analysis from dynamic contrast-enhanced MR imaging. European radiology. 2014;24(8):1914-1922.
5. Zha W, Nagle SK, Cadman RV, Schiebler ML, Fain SB. Three-dimensional Isotropic Functional Imaging of Cystic Fibrosis Using Oxygen-enhanced MRI: Comparison with Hyperpolarized 3He MRI. Radiology. 2019;290(1):229-237.
6. Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. Journal of thoracic oncology. 2011;6(2):244-285.
7. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. European respiratory journal. 2005;26(2):319-338.
8. Tustison NJ. Explicit B-spline regularization in diffeomorphic image registration. Frontiers in neuroinformatics. 2013;7:39.
9. Fedorov A, Beichel R, Kalpathy-Cramer J, et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magnetic resonance imaging. 2012;30(9):1323-1341.
10. Mäkinen JM, Laitakari K, Johnson S, et al. Nonpredominant lepidic pattern correlates with better outcome in invasive lung adenocarcinoma. Lung Cancer. 2015;90(3):568-574.
Figures