3187
A Novel Hybrid Score Integrating Clinical and MR Features to Predict Lumbar Vertebral Osteoporosis in Female
Shao-Chieh Lin1, Chun-Jung Juan2, Yi-Jui Liu3, Chun-Wen Chen4, Chien-Yuan Wang5, Wu-Chung Shen6, Der-Yang Cho7, and Kai-Yuan Cheng8
1Ph.D. program in Electrical and Communication Engineering, Feng Chia University, Taichung, Taiwan, 2Department of Medical Imaging, China Medical University Hsinchu Hospital, Hsinchu, Taiwan, 3Department of Automatic Control Engineering, Feng Chia University, Taichung, Taiwan, 4Department of Radiology, Taichung Armed Forces General Hospital, Taichung, Taiwan, 5Department of Orthopedics, China Medical University Hsinchu Hospital, Hsinchu, Taiwan, 6Department of Medical Imaging, China Medical University Hospital, Taichung, Taiwan, 7Department of Neurosurgery, China Medical University Hospital, Taichung, Taiwan, 8Department of Medical Imaging and Radiological Sciences, Central Taiwan University of Science and Technology, Taichung, Taiwan
1Ph.D. program in Electrical and Communication Engineering, Feng Chia University, Taichung, Taiwan, 2Department of Medical Imaging, China Medical University Hsinchu Hospital, Hsinchu, Taiwan, 3Department of Automatic Control Engineering, Feng Chia University, Taichung, Taiwan, 4Department of Radiology, Taichung Armed Forces General Hospital, Taichung, Taiwan, 5Department of Orthopedics, China Medical University Hsinchu Hospital, Hsinchu, Taiwan, 6Department of Medical Imaging, China Medical University Hospital, Taichung, Taiwan, 7Department of Neurosurgery, China Medical University Hospital, Taichung, Taiwan, 8Department of Medical Imaging and Radiological Sciences, Central Taiwan University of Science and Technology, Taichung, Taiwan
Synopsis
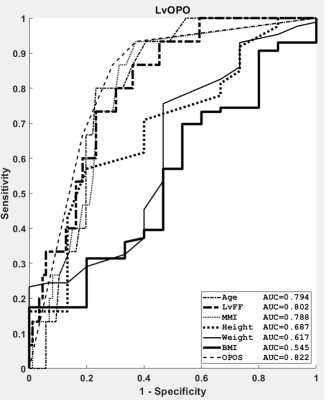
Lumbar vertebral osteoporosis (LvOPO) in women is clinically important. It is affected by mixed causes, including but not limited to the aging, lumbar vertebral fat fraction (LvFF), and estrogen. In the current study, the LvOPO in women was diagnosed by a newly proposed hybrid scoring system, i.e., the LvOPO score (LvOPOS). By integrating the independent predictors including age, LvFF, and menopause-MR interval (MMI), the LvOPOS achieved an AUC higher than the LvFF (0.802), age (0.794), and MMI (0.788). Our results provide a new insight in diagnosing the LvOPO specific to women with relevant to both clinical and MR features.
Introduction:
Lumbar vertebral osteoporosis (LvOPO) is a disease characterized by reduced bone mass and deteriorated bony micro-architecture of the lumbar vertebrae. LvOPO is defined as lumbar vertebral bone mineral density (BMD) of 2.5 standard deviations lower than the young adult reference mean [1]. A hybrid scoring system integrating clinical information and imaging features for diagnosing a certain disease is rapidly emerging. The increased of marrow fat deposition in the lumbar vertebrae was usually observed in the patients with reduced BMD [2]. Based on this observation, evaluation of lumbar vertebral fat fraction (LvFF) might play a role in better understanding LvOPO conceptually. Fat fraction has been successfully quantified using MRI in vivo, including but not limited to liver [3], parotid gland [4], and spine [5]. A hybrid scoring system integrating clinical information and imaging features for diagnosing a certain disease is rapidly emerging. For example, the Warthin tumor score been shown to outperform any independent predictors in diagnosing parotid Warthin tumors [6]. Such concept has not yet been applied to diagnose LvOPO. We hypothesized that hybrid scores integrating clinical and imaging features might also improve the diagnosis of LvOPO. The aim of our study was to propose a LvOPO score (LvOPOS) to diagnose LvOPO in postmenopausal women.Materials and Methods:
MRI study was performed using a 1.5T clinical scanner (Signa HDxt, GE Healthcare, Milwaukee, WI). Lumbar vertebral fat fraction (LvFF) was measured by quantitative magnetic resonance imaging using the iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL) method for fat-water quantification. Sagittal T2WI IDEAL fast spin echo (FSE-XL) imaging parameters included repetition time/echo time, 3000 ms/115.1 ms; receiver bandwidth, 63.86 kHz; echo train length, 20; field of view (FOV), 240 x 240 mm; slice thickness, 10 mm; matrix size, 320 x 192; number of excitations, 3; slice number, 3; flip angle, 90; . A total of 3 slices covered the lumbar spine from the T12 vertebra to the sacrum. Bone mineral density (BMD) of the lumbar spine, including L1 to L4 vertebrae, was measured by dual-energy X-ray absorptiometry (DeXA) using a Hologic QDR-4500W (S/N 47125) model (Hologic Inc., Bedford, MA, USA). BMD data were acquired, processed, and calculated based on the International Society for Clinical Densitometry (ISCD) guidelines [7].To represent the overall status of the BMD and fat fraction of each participant, the averaged BMD and LvFF was calculated by the L1 to L4 vertebrae. Statistical analyses were performed using MATLAB, SPSS Version 16.0 software (SPSS Inc, Chicago, III), and MedCalc Version 13.0 (MedCalc Software Inc, Ostend Belgium). The nonparametric receiver operating characteristics (ROC) curves were plotted and areas under curve (AUC) were calculated for distinguishing the LvOPO group from the normal group. Sensitivity, specificity, positive predictive value, negative predictive value, and overall accuracy of each predictor were calculated. A P value less than 0.05 was considered as statistically significant.Result:
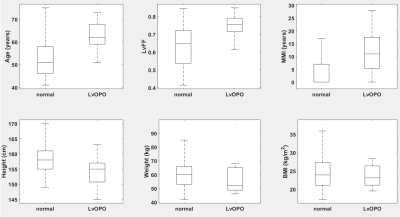
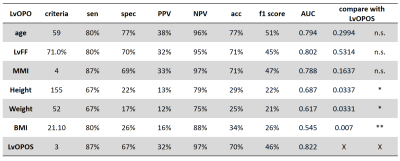
101 subjects after menopause were collected in this study. The LvOPO cases were 15 and normal subjects were 86. All participants received BMD measures using DXA as well as LvFF quantifications of using the IDEAL method. Clinical information including age, MMI, body height, body weight, body mass index (BMI) were recorded. Box and Whisker plots of the patient characteristics classified by the BMD were shown in Fig. 1. First, ROC curves of the clinical and imaging predictors in diagnosing the LvOPO were plotted in Fig. 2. The AUC of the age, LvFF, MMI, body height, body weight, and BMI in diagnosing the LvOPO was 0.794, 0.802, 0.788, 0.687, 0.617, and 0.545, respectively. Second, a parameter was selected as a predictor for the LvOPOS based on the criteria of an AUC no less than 0.7. Finally, the criteria allowing a sensitivity no less than 79%, together with highest specificity were selected for each predictor in the LvOPOS as listed in Table 1. The LvOPOS achieved the highest AUC (0.822), followed by the LvFF (0.802), age (0.794), and MMI (0.788) in diagnosing LvOPO.Discussion:
The difference of BMD can be attributed to the aging, which has an effect on bone loss via suppressing osteogenic programs in the bone marrow [8]. It can also be ascribed to the depletion of estrogen, which reduces bone resorption by inhibiting osteoclast formation and enhancing osteoclast apoptosis [9], in post-menopausal women. Our study showed a general trend of an inverse association between the BMD and LvFF as well as an inverse association between the BMD and age in the women. In addition, the LvOPOS is a good index with high AUC for diagnosing LvOPO in women.Acknowledgements
No acknowledgement found.References
- Sözen, Tümay et al. “An overview and management of osteoporosis.” European journal of rheumatology vol. 4,1 (2017): 46-56. doi:10.5152/eurjrheum.2016.048
- Schwartz, Ann V. “Marrow fat and bone: review of clinical findings.” Frontiers in endocrinology vol. 6 40. 30 Mar. 2015, doi:10.3389/fendo.2015.00040
- Kramer H, Pickhardt PJ, Kliewer MA, Hernando D, Chen GH, Zagzebski JA, et al. Accuracy of liver fat quantification with advanced ct, mri, and ultrasound techniques: Prospective comparison with mr spectroscopy. AJR Am J Roentgenol. 2017;208:92-100
- Chang HC, Juan CJ, Chiu HC, Liu YJ, Cheng CC, Chiu SC, et al. Parotid fat contents in healthy subjects evaluated with iterative decomposition with echo asymmetry and least squares fat-water separation. Radiology. 2013;267:918-923
- Chang R, Ma X, Jiang Y, Huang D, Chen X, Zhang M, et al. Percentage fat fraction in magnetic resonance imaging: Upgrading the osteoporosis-detecting parameter. BMC Med Imaging. 2020;20:30
- Wang CW, Chu YH, Chiu DY, Shin N, Hsu HH, Lee JC, et al. Journal club: The warthin tumor score: A simple and reliable method to distinguish warthin tumors from pleomorphic adenomas and carcinomas. AJR Am J Roentgenol. 2018;210:1330-1337
- Lewiecki EM, Gordon CM, Baim S, Leonard MB, Bishop NJ, Bianchi ML, et al. International society for clinical densitometry 2007 adult and pediatric official positions. Bone. 2008;43:1115-1121
- Kaiser J, Allaire B, Fein PM, Lu D, Jarraya M, Guermazi A, et al. Correspondence between bone mineral density and intervertebral disc degeneration across age and sex. Arch Osteoporos. 2018;13:123
- Manolagas SC. Birth and death of bone cells: Basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr Rev. 2000;21:115-137