3183
SEMI-AUTOMATIC QUANTIFICATION OF ABDOMINAL WALL MUSCLES DEFORMATIONS BASED ON DYNAMIC MRI IMAGE REGISTRATION1Aix-Marseille Univ, Univ Gustave Eiffel, IFSTTAR, LBA, Marseille, France, 2Aix Marseille Univ, CNRS, CRMBM, Marseille, France, 3Department of General Surgery, Aix Marseille Univ, North Hospital, APHM, Marseille, France
Synopsis
A novel semi-automatic post-processing method dedicated to real-time dynamic MRI aiming at a fast and reliable quantification of abdominal wall muscles deformations. The described method combines a highly accurate supervised 2D+t segmentation procedure of the abdominal wall muscles (mean Dice similarity coefficient of 0.95 ± 0.03), the quantification of muscles deformations based on masks registration and the mapping of deformations within muscle compartments leveraging a dedicated parcellation. The present genuine method provides a quantitative analytical frame that could be used in further studies for a better understanding of abdominal wall deformations in physiological and pathological situations.
INTRODUCTION
Real-time dynamic MRI is a promising modality in the field of medical imaging given its capacity to capture organs motion and deformation1–3. Although of interest, kinetic imaging of the abdominal wall is largely underused in clinical practice. More particularly, quantification of movement and deformations of abdominal muscles could bring valuable information in medical diagnosis and potentially shed light to better understand functional decline in certain neuromuscular diseases or any situations involving abdominal muscle deficiency. However the medical community is still lacking a standardized MRI protocol coupled with post-processing methods which would provide accurate and quantitative information that could be used by clinicians. A semi-automatic post-processing method dedicated to real-time dynamic MRI aiming at a fast and reliable quantification of abdominal wall muscles deformations during a controlled breathing exercise is reported.METHODS
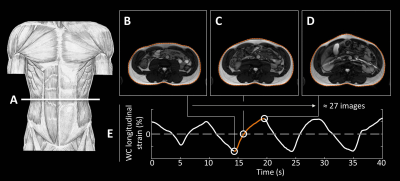
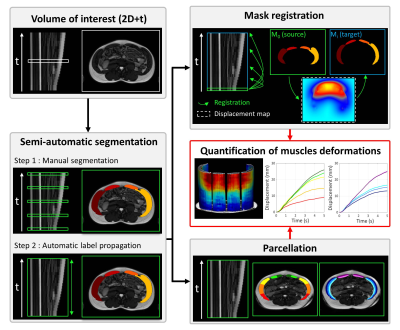
Ten healthy subjects (33.5 ± 10.8 y.o., 5 females) were imaged during a controlled breathing session at the L3-L4 disc level using real-time dynamic MRI at 3T. A coarse waist circumference (WC) feature tracking step allowed the selection of the inhalation cycle maximum abdominal excursion (figure 1).(i) Over the corresponding image series, the abdominal wall muscles were segmented using a supervised 2D+t segmentation procedure as illustrated in figure 2 (section B). For this purpose 5 slices were manually segmented and propagated to the remaining slices using an automatic label propagation algorithm4. The resulting segmentation was compared to the ground-truth manual segmentation based on the computation of Dice similarity coefficient (DSC) and the Hausdorff distance (HD).
(ii) The evolution over time of the displacement magnitude of the muscles compared to their initial position (i.e. end-exhalation) was computed from registration of the segmented masks as illustrated in figure 2 (section C). For this purpose, the first mask of the set M0 was consecutively registered toward each following masks Mi. The validity of the M0 to Mi registration, and consequently of the displacement magnitude calculation (figure, section E) was evaluated using the DSC and HD metrics computed between the registered M0 segmented mask and the corresponding target Mi segmented mask.
(iii) Finally, we mapped the displacement magnitudes within muscle compartments based on a dedicated automatic parcellation method as indicated in figure 2 (section D). A polar coordinate system was used to determine the position of each voxel of the segmented masks and to automatically split the muscles regions based on depth and angular constraints.
RESULTS
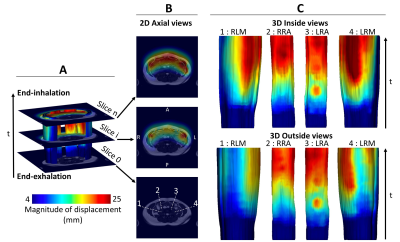
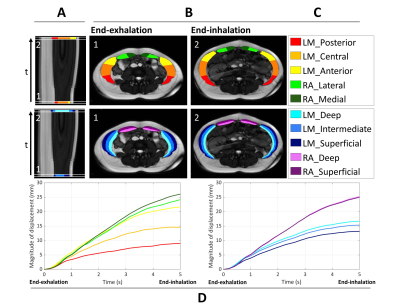
The DSC and HD metrics computed between the automatically-segmented slices and ground truth segmentation were respectively 0.95 ± 0.03 and 1.9 ± 1.1 mm. The DSC scores for the different muscle regions varied between 0.93 and 0.96. The HD values varied between 1.81 and 2.03 mm. The maps related to the magnitude of displacement resulting from mask registration are presented in figure 3 for a typical subject. The DSC and HD metrics computed between the registered source mask M0 and the target mask Mi were respectively 0.98 ± 0.01 and 2.1 ± 1.5 mm. From the magnitude of displacement maps, the time dependent change of the average displacement value within each parcel has been calculated and is shown in figure 4. Temporally, the magnitude of displacement evolved initially linearly and then was gradually stabilized towards the end of inhalation. Spatially, displacements greater than 26 mm were observed in the anterior area of the abdominal wall at end-inhalation, decreasing to less than 10 mm in the posterior areas. The parcellation of the lateral muscles highlighted the difference in displacement between the deep (16.7 mm) and superficial areas (13.2 mm).DISCUSSION
Applied on cine-BSSFP MRI data, our method allowed to quantify and localize spatially and temporally the abdominal wall muscles deformations during breathing. The accuracy of the semi-automatic segmentation procedure was supported by a very high DSC (0.95 ± 0.03) together with a very low HD (2.3 ± 0.7 mm) and was based on the manual delineation of only 20% of the data. The robustness of the displacement magnitude calculation was also supported by a very high DSC (0.98 ± 0.01) together with a very low HD (2.1 ± 1.5 mm) despite the large muscle deformations associated with inhalation. Parcellation allowed the attribution of displacement magnitudes to anatomically relevant muscle substructures which could not be distinguished on the basis of image contrast. The distribution of muscular displacements reported here supports the basic physiological knowledge regarding respiratory effort5,6 and the corresponding muscle activation7 and is in agreement previous studies reporting external measurements conducted at the abdomen surface8,9. 2D dynamic MRI might be considered as limited. However, this was necessary to achieve sufficient temporal resolution (182 ms) to correctly evaluate the dynamics of the exercise. In addition, it can be reasonably assumed that abdominal muscles displacements in the cranio-caudal direction are negligible and so because the muscular insertions on the bone rigid frame are likely to constrain the movements in the cranio-caudal direction.CONCLUSION
The present genuine post-processing method provides a quantitative analytical frame that could be used in further studies for the assessment of dysfunctions of the abdominal wall mobility and for a better understanding of abdominal wall deformations in physiological and pathological situations.Acknowledgements
We would like to thank Claire Costes, Lauriane Pini and Patrick Viout (CRMBM/CEMEREM UMR CNRS 7339) for their help in integrating the volunteers and carrying out the MRI acquisitions, Thomas Troalen (Siemens Healthineers) for his assistance in the optimization of the MRI sequences and Morgane Evin from (Gustave Eiffel University) for her help and insightful comments in the development of the features tracking algorithm.References
1. Kim RJ, Wu E, Rafael A, et al. The Use of Contrast-Enhanced Magnetic Resonance Imaging to Identify Reversible Myocardial Dysfunction. New England Journal of Medicine. 2000;343(20):1445-1453. doi:10.1056/NEJM200011163432003
2. Liu J, Wang Y, Wen Z, et al. Extending Cardiac Functional Assessment with Respiratory-Resolved 3D Cine MRI. Sci Rep. 2019;9(1):11563. doi:10.1038/s41598-019-47869-z
3. Comiter CV, Vasavada SP, Barbaric ZL, Gousse AE, Raz S. Grading pelvic prolapse and pelvic floor relaxation using dynamic magnetic resonance imaging. Urology. 1999;54(3):454-457. doi:10.1016/S0090-4295(99)00165-X
4. Ogier AC, Heskamp L, Michel CP, et al. A novel segmentation framework dedicated to the follow-up of fat infiltration in individual muscles of patients with neuromuscular disorders. Magnetic Resonance in Medicine. n/a(n/a). doi:10.1002/mrm.28030
5. Campbell EJM, Green JH. The variations in intra-abdominal pressure and the activity of the abdominal muscles during breathing; a study in man. J Physiol. 1953;122(2):282-290.
6. Mesquita Montes A, Baptista J, Crasto C, de Melo CA, Santos R, Vilas-Boas JP. Abdominal muscle activity during breathing with and without inspiratory and expiratory loads in healthy subjects. Journal of Electromyography and Kinesiology. 2016;30:143-150. doi:10.1016/j.jelekin.2016.07.002
7. Neumann P, Gill V. Pelvic Floor and Abdominal Muscle Interaction: EMG Activity and Intra-abdominal Pressure. Int Urogynecol J. 2002;13(2):125-132. doi:10.1007/s001920200027
8. Klinge U, Müller M, Brücker C, Schumpelick V. Application of three-dimensional stereography to assess abdominal wall mobility. Hernia. 1998;2(1):11-14. doi:10.1007/BF01207767
9. Song C, Alijani A, Frank T, Hanna GB, Cuschieri A. Mechanical properties of the human abdominal wall measured in vivo during insufflation for laparoscopic surgery. Surg Endosc. 2006;20(6):987-990. doi:10.1007/s00464-005-0676-6
Figures