3027
Disrupted Functional Connectivity of the Nucleus basalis of Meynert in Parkinson's Disease patients with Mild Cognitive Impairment1Department of Radiology, Xuzhou Medical University, Xuzhou, China, 2GE Healthcare,MR Research China, Beijing, China
Synopsis
Different functional connectivities of Basal nucleus of Meynert (BNM-FC) and the other brain regions among patients with Parkinson’s Disease (PD) accompanied and not accompanied with mild cognition impairment (PD-MCIs and PD-NCs, respectively) have been investigated in this study. A model based on Support-Vector-Machine with BNM-FC and neuropsychological results showed significantly decreased BNM-FC in the right superior parietal lobe of PD-MCIs than PD-NCs, allowing an accurate differentiation between PD-MCIs and PD-NCls. These results advanced our knowledge of the cholinergic system underpinning cognitive function in PD individuals.
Introduction
About 20%-40% patients with Parkinson’s diseases (PD) showed mild cognitive impairment (MCI) in the early stage 1. Basal nucleus of Meynert (BNM) is the main region of cholinergic innervation in the cerebral cortex 2. A large number of neuroimaging studies have reported that microstructural changes of BNM affected cognitive function. Resting state functional MRI (Rs-fMRI) provides the information of human brain connectomes noninvasively and satisfactory evidence of widespread abnormal cerebral connectivity in individuals with PD 3. To our best reviews, no applications of resting state-functional connectivity (rs-FC) on evaluation of the connectivity between BNM and the other brain regions in PD patients, and no combined applications of rs-FC and a supervised machine-learning approach to distinguish patients with PD accompanied with mild cognition impairment (PD-MCIs) from those without mild cognition impairment (PD-NCs) and healthy controls (HCs), have been reported so far. Therefore, in this study we aimed to confirm that PD-MCI has an abnormal FC between BNM and specific brain regions as we hypothesized.Materials and Methods
Subjects22 PD-MCI patients (mean age: 63.8 ± 9.3 years old), 22 PD-NC patients (mean age: 61.2 ± 8.7 years old) and 22 healthy controls (HCs) (mean age: 57.8 ± 6.4 years old) were recruited in this study for functional MRI scanning and neuropsychological tests. Written informed consent was obtained from each of them. MR Experiments All MRI experiments were performed on a 3T MR system scanner (Discovery 750w, GE Healthcare, USA) along with an 8 channel head and neck joint coil. Echo-planar imaging (EPI) sequence was used to acquire resting blood oxygen level dependent (BOLD) images. The scan parameters of BOLD were shown as follows: repetition time = 2000ms; echo time = 30 ms; slice thickness = 3 mm; slice gap = 1mm; total slices = 36; field of view = 220 mm × 220 mm; voxel size = 3.4 mm × 3.4 mm × 4.0 mm; flip angle = 90° and total volumes of each subjects was 185). The scan time was 6min 10s.
Data analysis
The rs-fMRI raw data were preprocessed using data Processing & Analysis for (Resting-State) Brain Imaging (DPABI) (http://www.rfmri.org/dpabi) including: slice timing, realignment, regression, normalization, filter and smoothing. Image data were excluded with head maximum displacement >2 mm, a maximum rotation >2.0°, or mean framewise displacement (FD) >0.3. 4 The BNM-FC between the seed BNM and all other brain regions were computed to generate correlation maps. FC was converted to z-value by fisher’s r-to-z transformation in order to improve normality at the group level analyses.5 Statistical analyses were performed using statistical parametric mapping 8. A general linear mode (GLM) with age, sex, and mean FD as covariates were used to compare the difference of BNM-FC between PD-MCI, PD-NC and HCs. Partial correlation analysis was then conducted to evaluate the relationship between these ROIs of BNM-FC and neuropsychological test scores controlling age and gender as covariates. Statistical significance was set at p<0.05 with Bonferroni correction for multiple comparisons. The group differences of BNM-FC were used as the classification features. The support vector machines (SVM) was used to model the training data with labeled observations,. Leave-one-out cross-validation (LOOCV) method was applied to estimate the generalization ability of the classifier. A permutation test was used to evaluate this classification accuracy.
Results
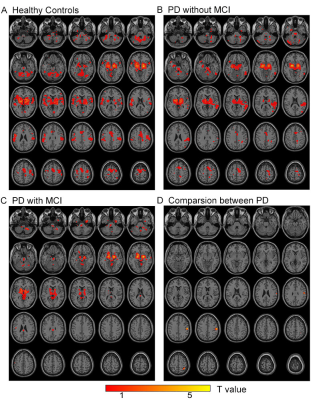
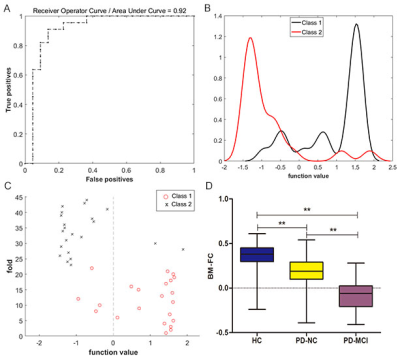
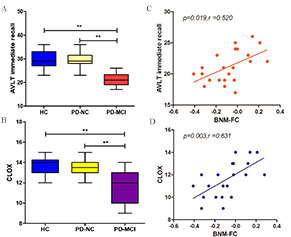
Significantly decreased BNM-FC values in the right superior parietal gyrus (SPL) and right postcentral gyrus were found in PD-MCI patients if compared with PD-NC patients and HCs (p<0.05, FDR correction) (Figure 1,2). Significantly positive correlation was found between BNM-FC in right SPL with AVLT immediate recall (r=0.520, p=0.019) and CLOX (r=0.631, p=0.003) scores in PD-MCI (Figure 3). The accuracy of linear SVM classifier using LOOCV achieved 86.36% (90.91% for sensitivity, 81.82% for specificity, p<0.001, nonparametric permutation approach) (Figure 2).Discussion and Conclusion
In this study, our findings were consistent with previous reports that BNM-FC in right SPL was crucial for maintaining short-term memory and visuospatial function. SVM showed a robust classification capability of distinguishing patients with PD-MCI from those with PD-NC using BNM-FC in the right SPL as the feature. To the best of our reviewing, no study reported that fasciculus in the direct or indirect fiber path from BNM to SPL can be visualized by the current MRI technique. This is the first study to investigate the BNM-FC in PD-MCI. Our study may provide novel insights on the pathophysiological mechanisms of PD-MCI. Future study of whether the observed cognitive impairment resulting from damaged white matter is associated with BNM with SPL will be implemented.Acknowledgements
The authors thank the patients in this study and the staff of the Department of Radiology for MRI data collection.References
1. Santangelo G, Vitale C, Picillo M, et al. Mild Cognitive Impairment in newly diagnosed Parkinson's disease: A longitudinal prospective study. Parkinsonism Relat Disord 2015;21(10):1219-1226.
2. Gratwicke J, Kahan J, Zrinzo L, et al. The nucleus basalis of Meynert: a new target for deep brain stimulation in dementia? Neurosci Biobehav Rev 2013;37(10 Pt 2):2676-2688.
3. Biswal B, Yetkin FZ, Haughton VM, et al. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med 1995;34(4):537-541.
4. Yan CG, Cheung B, Kelly C, et al. A comprehensive assessment of regional variation in the impact of head micromovements on functional connectomics. Neuroimage 2013;76:183-201.
5. Lowe SL, Francis PT, Procter AW, et al. Gamma-aminobutyric acid concentration in brain tissue at two stages of Alzheimer's disease. Brain 1988;111 ( Pt 4):785-799.
Figures