2987
The value of radiomics-based model on contrast-enhanced MRI for predicting microvascular invasion in HCC before Partial Hepatectomy1Department of Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2GE Healthcare, Beijing, China
Synopsis
Hepatocellular carcinoma (HCC), often occurring in patients with chronic viral hepatitis and cirrhosis, was one of the most common malignant tumors. Microvascular invasion (MVI) is one of the well-known potential predictors related to the prognosis of HCC. MVI with higher positive expression indicates more aggressive behaviour of HCC and poorer survival outcomes. Early accurate prediction for MVI status plays an important guiding role in surgical selection and adjuvant therapy for HCC. We proposed a radiomics model based on enhanced MRI to predict MVI in HCC before surgery.
Introduction
Hepatocellular carcinoma (HCC), often occurring in patients with chronic viral hepatitis and cirrhosis, was one of the most common malignant tumors[1]. Surgical resection is currently the most effective treatment, however, the high incidence of recurrence remained a major challenge after surgical resection. Microvascular invasion (MVI) is one of the well-known potential predictors related to the prognosis of HCC. MVI with higher positive expression indicates more aggressive behaviour of HCC and poorer survival outcomes[2]. Early accurate prediction for MVI status plays an important guiding role in surgical selection and adjuvant therapy for HCC[3]. We proposed a radiomics model based on enhanced MRI to predict MVI in HCC before surgery.Materials and Methods
Our study included a training cohort of 77 HCC patients and a validating cohort of 34 HCC patients, who underwent preoperative enhanced MRI examination and curative hepatectomy. MRI was performed using a 1.5-T MR imager (GE-Signa HDXT). All underwent contrast-enhanced MR examinations within two weeks before Partial Hepatectomy. The volumes of interest (VOIs) were delineated around the liver lesions outline for 3D volume area as indicated MRI images by two independent radiologists with more than 5 years of experience with ITK-Snap software. The features were extracted by the A.K. software (Analysis-Kit, GE Healthcare). A total of 1044 imaging features were extracted. Spearman correlation and Least absolute shrinkage and selection operator logistic regression was applied to select features and construct signatures derived from combined arterial phase, venous phase, and delay phase MR images. Then, logistic regression was applied to construct a prediction radiomics-based model. Receiver operating characteristic (ROC) curve was performed to determine the performance of the model; and accuracy, sensitivity, specificity and area under curve (AUC) were calculated. Decision curve analysis was conducted to determine the clinical usefulness of radiomics-based model. All statistical analyses for the present study were performed with R 3.5.1 and Python 3.5.6. A two-tailed p-value <0.05 indicated statistical significance.Result
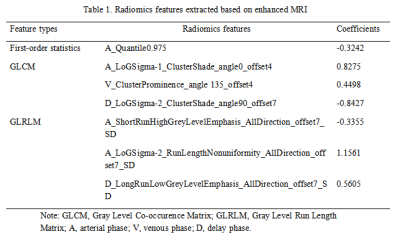
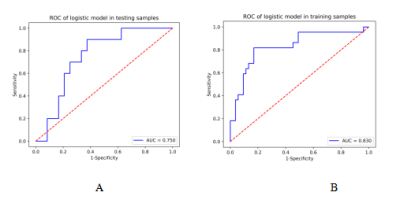
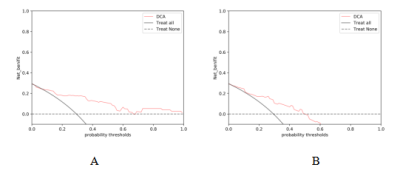
In the whole cohort, 34 patients were MVI positive and 75 patients were MVI negative. Ultimately, 7 radiomics features, which were showed in Table 1, were selected to construct a prediction radiomics-based model using logistic regression . The AUC, sensitivity, specificity of the radiomics model in the training and test cohort were 0.83, 63.6%, 88.7% and 0.75, 50%, 79.2%. the sensitivity were 63.6%, 50%, respectively (Figure 1). Decision curves confirmed that our model achieved good clinical utility (Figure 2).Discussion and conclusion
Radiomics, based on quantitative image analysis, reflected image textures and morphology of tumours by grey value[4]. Compared with conventional quantitative parameter analysis, radiomics was objective and accurate. We provide and validate an effective radiomics-based model for predicting MVI in HCC patients, and may help clinicians make precise decisions regarding treatment before the surgery of HCC patients.Acknowledgements
None.References
[1] Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012 , 379(9822): 1245-55.
[2] LimKC, ChowPK, Allen JC et al. Microvascular invasion is a better predictor oftumour recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to the Milan criteria. Ann Surg, 2011, 254:108–113.
[3] Yang L, Gu D, Wei J, et al. A Radiomics Nomogram for Preoperative Prediction of Microvascular Invasion in Hepatocellular Carcinoma. Liver Cancer, 2019, 8: 373-386.
[4] Feng ST, Jia Y, Liao B et al. Preoperative prediction of microvascular invasion in hepatocellular cancer: a radiomics model using Gd-EOB-DTPA-enhanced MRI. Eur Radiol, 2019, 29: 4648-4659.
Figures