2908
Cardiac Magnetic Resonance and hemodynamic predictors of postoperative Fontan Outcomes
Jyothsna Akam Venkata1,2, Mohamed Abdelghafar Hussein1,3, Joshua Greer1, Robert Jaquiss4, Gerald Greil1, Jeanne Dillenbeck1, Surendrenath R Veeram Reddy 1, Jenifer Hernandez1, and Tarique Hussain1
1Dept of Pediatrics, Division of Pediatric Cardiology, UT Southwestern Medical Center, Dallas, TX, United States, 2University of Mississippi Medical Center, Jackson, MS, United States, 3Kafrelsheikh University, Kafr Elsheikh, Egypt, 4Department of Pediatric Cardiothoracic Surgery, UT Southwestern Medical Center, Dallas, TX, United States
1Dept of Pediatrics, Division of Pediatric Cardiology, UT Southwestern Medical Center, Dallas, TX, United States, 2University of Mississippi Medical Center, Jackson, MS, United States, 3Kafrelsheikh University, Kafr Elsheikh, Egypt, 4Department of Pediatric Cardiothoracic Surgery, UT Southwestern Medical Center, Dallas, TX, United States
Synopsis
Pre-Fontan cardiac assessment with CMR in conjunction with cardiac catheterization has increasingly become the standard of care. Cardiac catheterization and CMR performed for pre-Fontan assessment at a single institution between April 2017 and June 2020 were analyzed. Our cohort consisted of 43 patients with median age of 3.7 years(range 1.8-14) at the time of CMR. Median age at Fontan operation was 4 years (2.4-14). We found significant correlation between CMR derived ventricular end diastolic, end systolic volume, ejection fraction and cardiac catheterization derived ventricular end-diastolic and mean superior vena cava pressure, and duration of post-operative hospital stay after Fontan operation.
Introduction
Pre-Fontan cardiac assessment with CMR in conjunction with cardiac catheterization has increasingly become the standard of care. CMR is increasingly comprehensive including assessment of systemic ventricular volumes, systolic function, anatomy, atrioventricular valve regurgitation (AVVR), branch pulmonary artery anatomy with flow distribution, lymphatic system abnormalities, burden of collateral blood flow and sternal adhesions. We sought to evaluate the incremental value of novel CMR evaluation for post-operative Fontan outcomes.Methods
Cardiac catheterization and CMR exams performed for pre-Fontan assessment at a single institution between April 2017 and June 2020 were analyzed. Sequences of CMR included (i) balanced 2D Steady-state free precision cine imaging to calculate ventricular end-diastolic, end-systolic volume, ejection fraction, (ii) phase-contrast imaging to estimate flow to the pulmonary and systemic circulation (Qp:Qs), (iii) T2 weighted turbo-spin echo sequence to assess the lymphatic system1 (iv) 3D-SSFP (v) 3D-black blood VISTA to assess the anatomy of the pulmonary arteries, aorta, systemic and pulmonary veins, and (vi) real-time cine with free-breathing to assess for retro-sternal adhesions. Lymphatic abnormality was classified into grades 1-4 according to Dori et al2. Maldistribution of pulmonary blood flow was classified as flow discrepancy greater than 70: 30% to both the lungs. Pulmonary vascular resistance (PVR) was calculated from cardiac catheterization derived transpulmonary gradient divided by phase-contrast derived pulmonary blood flow. Atrioventricular valve regurgitation was estimated as the ratio of (systemic ventricular stroke volume- aortic or neo-aortic valve forward flow)/ventricular stroke volume3. Surgical details and the immediate post-operative outcomes such as adverse outcomes, duration of hospital stay, chylous effusion, re-admissions were reviewed. Adverse outcomes included cardiac arrest, extracorporeal membranous oxygenation support, the takedown of Fontan circulation, mechanical support (VAD-ventilator assist device), heart transplantation, or death. CMR and hemodynamic parameters were compared between groups with adverse and favorable outcomes. The study was approved by the institutional review board. SPSS v.22 was used for Statistical analysis.Results
A total of 56 CMR exams were performed for pre-Fontan assessment, of which 13 patients are awaiting Fontan operation. Our final cohort consisted of 43 patients (29 males) with a median age of 3.7 years (range 1.8-14) at the time of CMR. The median age at Fontan operation was 4 years (2.4-14). 40 patients underwent extra-cardiac conduit placement (39 fenestrated). 2 Patients underwent biventricular conversion. 6 patients had adverse outcomes (including 2 undergoing transplantation or VAD prior to Fontan). Pre-Fontan systemic ventricular ejection fraction (EF), (r=-0.56, p=0.004), ventricular end diastolic volume (EDV) (r=+0.74,p<0.001), end systolic volume(ESV) (r=+0.8, p<0.001), systemic ventricular end-diastolic pressure (EDP) (r=+0.611, p<0.002) and mean superior vena cava (SVC) pressure (r=+0.69, p<0.001) significantly correlated with duration of post-Fontan hospital stay. Patients with adverse outcomes had a tendency for higher collateral blood flow (median 22.5%, range 3-40 vs 8.5%,0-27, p-0.06) but no factors significantly predicted adverse outcome. Factors such as AVVR, aortic arch patency, the ratio of pulmonary to systemic arterial blood flow (Qp: Qs), maldistribution of pulmonary blood flow, pulmonary vascular resistance (PVR), the grade of lymphatic abnormality were not predictive of the length of postoperative stay. There was no significant correlation between lymphatic classification and post-operative chylous effusion (p=0.786) or readmission (p=0.277). Grade 4 (n=1) lymphatic abnormality was associated with death after Fontan. Retrosternal adhesions were present in 87% of the patients.Discussion
This CMR approach provides a comprehensive assessment of the single ventricle physiology and anatomy in combination with cardiac catheterization data to assess ventricular function, branch pulmonary artery anatomy, flow distribution, lymphatic abnormalities, retro-sternal adhesions, and bleeding risk in the pre-operative Fontan assessment. We found a significant correlation between the CMR derived ventricular end-diastolic, end-systolic volume, ejection fraction, and cardiac catheterization derived ventricular end-diastolic pressure and mean superior vena cava pressure and duration of postoperative hospital stay after Fontan operation. Those with adverse outcomes tended to have a higher collateral burden compared to those with favorable outcomes. We did not find significant correlation between the ratio of pulmonary to systemic blood flow (Qp: Qs), maldistribution of pulmonary blood flow, pulmonary vascular resistance, the grade of lymphatic abnormality, AV valve regurgitation, and postoperative outcomes.Conclusion
Pre-Fontan CMR derived systemic ventricular EF, ventricular EDV and ESV along with cardiac catheterization derived ventricular EDP and mean SVC pressure are useful measures in predicting the duration of post-Fontan hospital stay.Acknowledgements
No acknowledgement found.References
- Pamarthi V, Pabon-Ramos WM, Marnell V, Hurwitz LM. MRI of the Central Lymphatic System: Indications, Imaging Technique, and Pre-Procedural Planning. Top Magn Reson Imaging. 2017 Aug;26(4):175-180. doi: 10.1097/RMR.0000000000000130. PMID: 28665889; PMCID: PMC5548502.
- Biko DM, DeWitt AG, Pinto EM, Morrison RE, Johnstone JA, Griffis H, O'Byrne ML, Fogel MA, Harris MA, Partington SL, Whitehead KK, Saul D, Goldberg DJ, Rychik J, Glatz AC, Gillespie MJ, Rome JJ, Dori Y. MRI Evaluation of Lymphatic Abnormalities in the Neck and Thorax after Fontan Surgery: Relationship with Outcome. Radiology. 2019 Jun;291(3):774-780. doi: 10.1148/radiol.2019180877. Epub 2019 Apr 2. PMID: 30938628; PMCID: PMC6542623.
- Garg P, Swift AJ, Zhong L, Carlhäll CJ, Ebbers T, Westenberg J, Hope MD, Bucciarelli-Ducci C, Bax JJ, Myerson SG. Assessment of mitral valve regurgitation by cardiovascular magnetic resonance imaging. Nat Rev Cardiol. 2020 May;17(5):298-312. doi: 10.1038/s41569-019-0305-z. Epub 2019 Dec 9. PMID: 31819230; PMCID: PMC7165127.
Figures
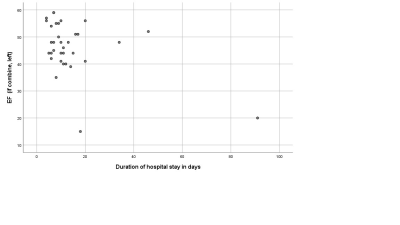
Correlation between single ventricular ejection fraction and post-operative hospital stay after Fontan operation.
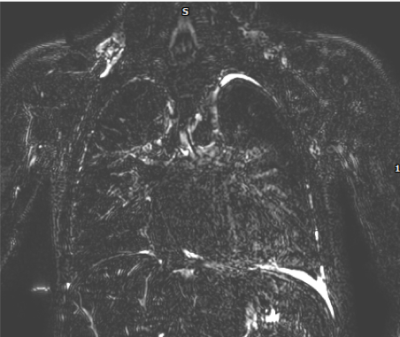
T2 weighted turbo spin echo sequence showing grade 4 DORI classification of lymphatic abnormality (lymphatic leak in the bilateral supraclavicular, mediastinal lymph nodes and into the interstitium of the lung parenchyma).
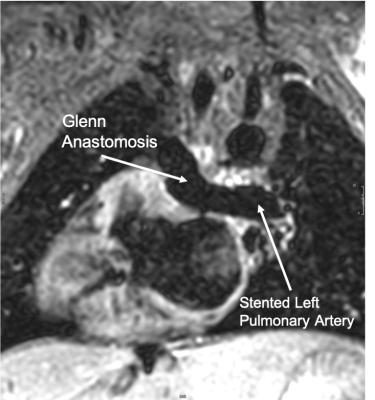
3D volume isotropic turbo spin-echo acquisition (VISTA) sequence showing the bidirectional Glenn anastomosis and the stented left pulmonary artery without stent artifact in a single ventricle patient with Dextrocardia.