2898
Whole heart coronary MRA using image-based 2D navigator (iNav) and conventional Nav system: comparison of image quality and scan time
Kazuo Kodaira1, Michinobu Nagao2, Masami Yoneyama3, Yasutomo Katsumata3, Takumi Ogawa1, Yutaka Hamatani1, Isao Shiina1, Yasuhiro Goto1, Mamoru Takeyama1, Isao Tanaka1, and Shuji Sakai2
1Department of Radiological Services, Tokyo Women's Medical University Hospital, tokyo, Japan, 2Department of Diagnostic imaging & Nuclear Medicine, Tokyo Women's Medical University Hospital, tokyo, Japan, 3Philips Japan, tokyo, Japan
1Department of Radiological Services, Tokyo Women's Medical University Hospital, tokyo, Japan, 2Department of Diagnostic imaging & Nuclear Medicine, Tokyo Women's Medical University Hospital, tokyo, Japan, 3Philips Japan, tokyo, Japan
Synopsis
Diaphragmatic one-dimensional navigation (NAV) is the conventional approach for CMRA respiratory motion compensation. This method has limitations such as the cumbersomeness of setting NAV and giving stresses to patients by wrapping the compression band around the chest/abdomen for minimizing respiratory artifacts. Image-based 2D navigator (iNAV) can solve this limitation because it directly corrects the translational movement of the heart in two directions (R-L and F-H) by using 2D real-time imaging. We investigate the feasibility of iNAV with loosely wrapped abdominal compression band compared to the conventional NAV approach.
Introduction
The sequences of various methods have been proposed for whole heart coronary magnetic resonance angiography (WHC-MRA)1-4. In conventional WHC-MRA, it is typically performed during free-breathing, and respiratory motion is prospectively compensated by using a 1D-right-diaphragmatic-navigator (NAV), measuring motion in the FH-direction5. However, the limitations of the NAV-method are the cumbersomeness of setting the NAV on the right-diaphragm and giving stresses to patients by wrapping the compression-band around the chest/abdomen for minimizing respiratory artifacts. Image-based-2D-navigator (iNAV) has the possibility to solve these problems. The iNAV allows prospective correction of translational motion of the heart in two-directions (R-L, F-H) by using 2D-real-time imaging to track the region surrounding the coronary arteries throughout the cardiac cycle5 (Fig. 1-2). Furthermore, this method allows direct motion estimation and correction of respiratory induced motion of the heart, obviating the need for a diaphragmatic motion model6. Consequently, the iNAV enables more robust suppression of respiratory motion artifacts for WHC-MRA compared with conventional NAV, and images can be acquired in shorter time and with improved image quality5-7. Therefore, by using iNAV, we hypothesized that the image quality of WHC-MRA can be maintained while shortening the scan time even if the abdominal compression-band is loosened. In this study, we investigated the feasibility of iNAV with a loosely wrapped compression-band for WHC-MRA by comparing it with conventional NAV.Methods
A total of six volunteers (6 males; age range: 23~44) were examined on a 1.5T MRI (Ingenia CX, Philips Healthcare). The study was approved by the local IRB, and written informed consent was obtained from all subjects. We used 3D-balanced-TFE (bTFE) for WHC-MRA images. Using bTFE as a base sequence, we compared NAV-approach and iNAV-approach with loosely or tightly wrapped abdominal compression-band (NAV-loose/NAV-tight/iNAV-loose/iNAV-tight). For iNav scans, motion corrections for both head-foot and left-right directions were enabled. For respiratory gating in iNav, we applied Constant Respiratory efficiency UsIng Single End-expiratory threshold (CRUISE) algorithm8. CRUISE assumes a fixed scan efficiency of 50%. Therefore, the total scan time will be exactly double of the displayed time. The imaging-parameters of bTFE: FOV=300×300mm, voxel-size=1.6×1.6×1.6mm, SENSE-factor=2.4, TR/TE/FA=2.2/1.1/80. Scan time was recorded for each sequence. Image quality was evaluated by visual score at the 10-points (RCA: #1/2/3/4 LAD: #5/6/7/8 CX: #11/13) based on American-Heart-Association classification. We evaluated them as 4-point grades (grade “4” was excellent, “1” was severe) by two blinded readers. For quantitative comparison, signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) were measured. The SNR was assessed in the blood, epicardial fat and myocardium. To allow quantitative SNR measurements, we used a noise-measurement-method proposed by Zwanenburg et al9. Each sequence was repeated with exactly the same receiver gain, but without any RF and gradient-pulses. The reconstructed images showed only noise, including the noise added due to the SENSE-reconstruction. The standard-deviation of a region of interest of the corresponding area in the noise image was used as metric for the noise. SNRblood, SNRepicardial fat and SNRmyocardium were then calculated as follows: SNRA = SI(A) / SDnoise(A) Where SI are the mean average signal intensity of the blood, epicardial fat and myocardium respectively, and the corresponding SDnoise is the standard-deviation at the same location on the noise images. Subsequently, we measured the CNR for comparing image contrast quantitatively. The CNR was estimated for blood and epicardial fat (CNRblood-epicardial fat). The CNRblood-epicardial fat was calculated by the following equations: CNRA-B = [SI(A) - SI(B)] / 0.5 [SDnoise(A) + SDnoise(B)] The SNR and CNR were assessed by one-way repeated measures analysis of variance (ANOVA) and the post- hoc Tukey-Kramer test.Results
Figure 3 shows the representative images using NAV-loose, NAV-tight, iNAV-loose and iNAV-tight. The results of visual score and average scan time are shown in Figure 4. The iNAV-approach showed significantly higher than NAV-approach regarding RCA, LAD, except for the comparison between NAV-tight and iNAV-loose. Regarding CX, there was no significant difference in the comparison of all sequences. Average scan time was significantly shorter iNAV-approach compared with NAV-approach, except for the comparison between NAV-tight and iNAV-loose. Figure 5 shows SNR and CNR comparison among four sequences. For the SNRblood, there was no significant difference in the comparison of all sequences. For the SNRepicardial fat, iNAV-approach showed significantly lower value compared to NAV-approach. For the SNRmyocardium, there was no significant difference in the comparison of all sequences. For the CNRblood-epicardial fat, iNAV-approach showed significantly lower value compared to NAV-approach.Discussion
From the results of SNR and CNR, it is considered that iNAV-approach has a better contrast between arteries and background fat tissues than NAV-approach. We considered that iNAV-approach has higher fat suppression effect than NAV-approach because the additional SPIR-pulse in the iNAV might affect the results of fat suppression. Therefore, it is considered that iNAV-approach showed a higher value in the visual score than NAV-approach.Conclusion
By using iNAV for WHC-MRA, image quality could be maintained without tightly wrapping the abdominal compression-band, and the scan time could be shortened compared to the conventional NAV-approach. Therefore, iNAV can reduce patients’ stress. In addition, iNAV eliminates the cumbersomeness of setting the NAV on the right diaphragm, reducing the burden on the scanner. Therefore, iNAV could improve the workflow of WHC-MRA.Acknowledgements
No acknowledgements found.References
(1) Kazuo Kodaira, et al. Whole heart coronary MRA with 3D non-selective bSSFP-DIXON: comparison with conventional methods. Proceedings of the Virtual Conference & Exhibbition of ISMRM (2020). (2) Oliver M. Weber, PhD et al. Free-Breathing, Three-Dimensional Coronary Artery Magnetic Resonance Angiography: Comparison of Sequences. Journal of Magenetic Resonance Imaging. 2004; 20: 395-402. (3) Yuji Iyama et al. Single-Breath-Hold Whole-heart Unenhanced Coronary MRA Using Multi-shot Gradient Echo EPI at 3T: Comparison with Free-breathing Turbo-field-echo Coronary MRA on Healthy Volunteers. Magn Reson Med Sci. 2018; 17: 161-167. (4) Teresa Correia et al. Technical note: Accelerated nonrigid motion-compensated isotropic 3D coronary MR angiography. Med Phys. 2018 Jan; 45(1): 214-222. (5) Markus Henningsson et al. Prospaective Respiratory Motion Correction for Coronary MR Angiography Using a 2D Image Navigator. Magn Reson Med. 2013; 69: 486-494. (6) Markus Henningsson et al. Whole-Heart Coronary MR Anigiography Using Image-Based Navigation for the Detection of Coronary Anomalies in Adult Patients With Congenital Heart Disease. Journal of Magenetic Resonance Imaging. 2016; 43(4): 947-955. (7) Markus Henningsson et al. Whole-Heart Coronary MR Angiography With 2D Self-Navigated Image Reconstruction. Magn Reson Med. 2012; 67: 437-445. (8) Markus Henningsson et al. Coronary MR Angiography Using Image-Based Respiratory Motion Compensation With Inline Correction and Fixed Gating Efficiency. Magn Reson Med. 2018; 79: 416-422. (9) Zwanenburg et al. MR Angiography of the cerebral perforating arteries with magnetization prepared anatomical reference at 7T: comparison with time-of-flight. J Magn Reson Imaging. 2008; 28: 1519–1526.Figures
Figure
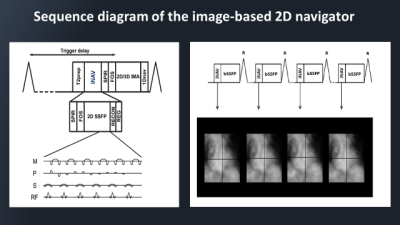
1: Sequence diagram of the iNAV used for prospective motion correction. The iNAV
uses fat suppression (SPIR) and fold-over suppression (FOS), to suppress signal
from epicardial fat and to reduce fold-over artifacts. Reconstruction (RECON)
and image registration (REG) are performed immediately after iNAV acquisition,
which yields displacement information in FH and LR direction and is used for
slice tracking. The iNAV can be combined with 2D or 3D gradient echo-based
imaging sequences (2D/3D IMA). iNAV images were generated in every cardiac
cycle.
Figure
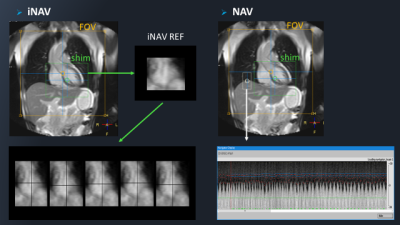
2: Scan planning of WHC-MRA with iNAV/NAV approach. Both sequences were coronal orientation,
with shim geometry covering the whole heart. The iNAV image is a projection of
the shim area, and the first acquired iNAV image is reference navigator (iNAV
REF). To extract respiratory motion, the optimal location of iNAV REF in
subsequent iNAV images was determined by finding the pixel with maximum
normalized cross-correlation between the images. In the NAV-approach, the 1D
navigator ROI is set on the diaphragm. Only expiratory phase data is applied
from the data obtained from NAV.
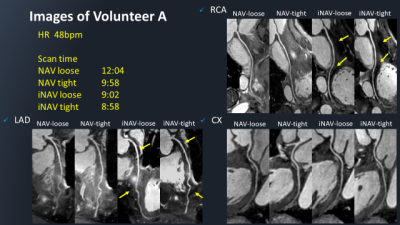
Figure 3: CPR images of coronary
artery of volunteer A in NAV approach and iNAV-approach. Compared to NAV-approach,
iNAV-approach has a better
contrast between arteries and background fat tissues regarding RCA and LAD. The
distal blood vessels are more visible. Moreover, iNAV has more accurate motion correction
and higher sharpness than NAV.
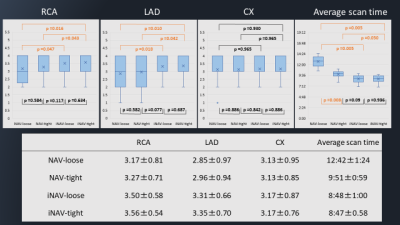
Figure
4: The results of visual score and scan
time. In
visual score, iNAV-approach showed higher overall than
NAV-approach. The iNAV-approach showed significantly higher than NAV-approach regarding
RCA, LAD, except for the comparison between NAV-tight and iNAV-loose. Regarding CX, there was no significant
difference in the comparison of all sequences. In scan time, iNAV-approach was shorter
than NAV-approach and was independent of abdominal
compression band tightness.
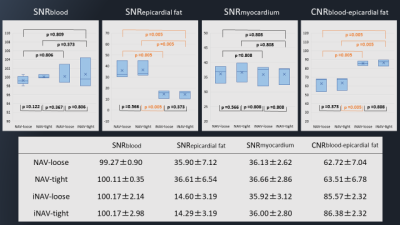
Figure
5: The results of SNR and CNR. For the SNRblood,
there was no significant difference in the comparison of all sequences. For the
SNRepicardial fat, iNAV-approach showed significantly
lower value compared to NAV-approach. For the SNRmyocardium,
there was no significant difference in the comparison of all sequences. For the
CNRblood-epicardial fat, iNAV-approach showed significantly
lower value compared to NAV-approach.