2896
Clinical impact of compressed sensing on whole-heart coronary MRI1MRI department, Wuhan Asia Heart General Hospital, WuHan, China, 2philips, healthcare, Beijing, China
Synopsis
Diagnosis of Coronary artery disease using MRI remains a challenge due to the long scan times, limited spatial resolution, and low signal-to-noise of MRI technique. Compressed Sensing (CS) is a novel technique to accelerate the imaging and improve detection of coronary stenosis by coronary MRI. Results of this study indicate that there was no statistical difference in coronary artery image quality from the scanning with CS acceleration factors (AF) of 2, 4, 6. Since CS AF of 6 provides the shortest scan time and favorable image quality, this might be an optimal setting for clinical whole-heart coronary MRI.
Introduction
Coronary artery disease remains the leading cause of death in recent decades1. There have been fast-growing demands for non-invasive coronary evaluation, particularly medical imaging. Compared with DSA and CT, coronary MRI has the advantage of non-invasive and contrast agent-free. However, long acquisition time, low signal-to-noise-ratio, and high rate of acquisition failure still limit its routine clinical application, especially when the patient coordinations are challenging for the examination. Compressed sensing (CS), as a relatively novel imaging acceleration technique, has been increasingly studied for its feasibility and optimal setups in clinical scenarios2. In this work we evaluated the performance of whole heart clinical coronary MRI accelerated by CS with different acceleration factors (AF).Methods
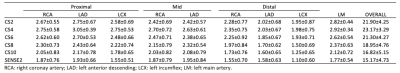
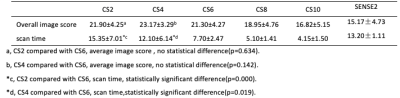
This study was approved by the institutional IRB. Twenty healthy volunteers (mean age: 51±16 years, range:28-74 years; 11 men,9 women) were recruited with written informed consent acquired from each subject. All volunteers were scanned using a 1.5T MR system (Ambition, Philips Healthcare, the Netherlands) with a 32-channel body coil. The MR protocols with SENSE AF of 2 and CS AFs of 2,4,6, 8, and 10 were based on a free-breathing electrocardiogram-triggered navigator-gated steady-state free precession sequence. The electrocardiogram trigger delay was identified by visualizing the quiescent period of the right coronary artery (RCA) using a 100 phases breath-hold cine image in the two chamber view (temporal resolution 7.5 ms)2. All other parameters were kept the same (TR/TE = 4.3/2.1ms, FOV = 320x279x120 mm3, Matrix = 212x186x160, Voxel= 1.5×1.5×1.5 mm3, flip angle = 90°). The total 6 examinations were implemented in random orders for each patient, in case the results were affected by the state of patients during the long acquisition (about 1 hour). The image quality was assessed on a four-point scale(1=poor,2=fair,3=good,4=excellent)3 with the following criteria 1, coronary artery visible, with remarkably blurred borders and edges; 2, coronary artery visible, with moderately blurred borders and edges; 3, coronary artery visible, with mildly blurred borders and edges; 4, coronary artery visible, with sharply defined borders and edges. Three radiologists evaluated the image quality by subjective scores independently (Table 1). As the data was in the normal distribution, the repeated measure ANOVA test was employed to assess the image quality difference between CS AF of 2, 4, 6, 8, 10 and SENSE AF of 2 in image scores. Since the scan time was affected by the heart rate and breathing state of the individual patient, we also analyzed the scan time of different acceleration schemes.Results
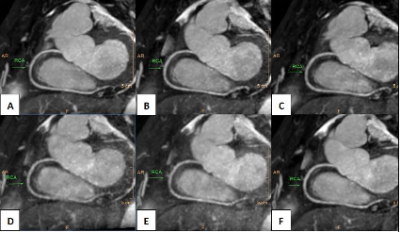
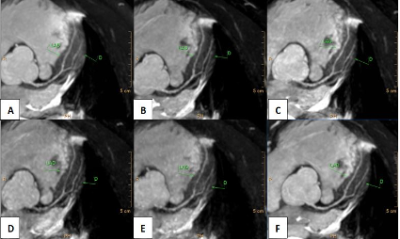
The representative images of the right coronary artery and left coronary artery with different acceleration schemes were shown in Figure 1 and Figure 2. The coronary artery branches image quality scores were in Table 1. The quality score of images with CS AF of 2,4, and 6 were significantly higher than CS AF of 8, 10 and SENSE AF of 2 based on analysis of scoring of nine coronary arteries (p <0.05, Table 2). There was no statistical difference between acceleration schemes of CS AF of 2, 4, 6 in image quality. The scan time of images with CS AF of 6 was statistically shorter than that of images with CS AF of 2 and 4.Discussion
Despite the shortened imaging time, the image quality was reduced when the CS AF went beyond 6. On the other hand, when compared to the SENSE AF 2, CS 6 yielded significantly better image quality in coronary MRI, while reducing the scan time to approximately 7 minutes (a cut of 42%) which is feasible in clinical applications. Therefore, this setting might be an optimal balance of image quality and scan time for whole-heart coronary MRI.Conclusion
In conclusion, this study demonstrates that CS accelerated whole-heart coronary MRI with AF of 6 could achieve good image quality and reduce the scan time significantly, which suggested it a promising and valuable non-invasive clinical method for the diagnosis of coronary artery disease.Acknowledgements
On this occasion there is no one we wish to acknowledgement.References
1. Zhou, M. et al. Cause-specific mortality for 240 causes in China during 1990-2003: a systemic subnational analysis for the Global Burden of Disease Study 2013. Lancet 387, 257-272(2016).
2. Akcakaya M, Basha TA, Chan RH, et al. Accelerated Isotropic Sub-Millimeter Whole-Heart Coronary MRI: Compressed Sensing Versus Parallel Imaging. Magn Reson Med. 2014;71(2):815-822.
3. Kim WY, Danias PG, Stuber M, et al. Coronary magnetic resonance angiography for the detection of coronary stenosis. N Engl J Med 2001;345:1863-1869.
Figures