2894
Improved free-breathing zoomed whole heart coronary MRA using 3D stack-of-stars radial sequence with diamond pseudo-golden angle sampling1radiology, Tokyo metropolitan police hospital, Tokyo, Japan, 2Philips Japan, Tokyo, Japan, 3Tokyo metropolitan police hospital, Tokyo, Japan
Synopsis
One of the problems of whole heart coronary MRA is the prolongation of acquisition time, and the radial sampling technique is able to obtain the image of inconspicuous artifacts such as aliasing and motion. Furthermore, the improved sequence of 3D d-Vane is possible to adopt a self-navigator without extend scan time. Hence the small FOV whole heart coronary MRA with diamond pseudo golden angle radial sampling showed improved efficiency with maintaining the image quality.
Introduction
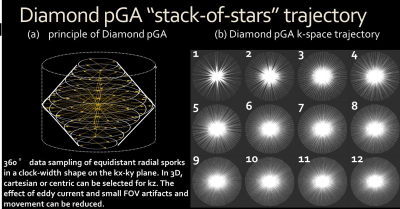
Small-FOV 3D stack-of-stars radial sequence (3D Vane) has been used to obtained free-breathing zoomed whole heart coronary MRA (WHC-MRA) without respiratory navigator gating or extended scan time while preventing aliasing and motion artifacts. Recently, another 3D stack-of-stars radial sequence with diamond pseudo-golden angle radial sampling (3D d-Vane) and the self-respiratory gating has been developed for free-breathing coronary imaging. In this study, we demonstrate the feasibility of zoomed WHC-MRA with self-respiratory gating using 3D d-Vane combined with bSSFP.Methods
Using our institutional review board-approved procedures, 6 volunteers underwent volunteer examination using a 1.5T Philips MR system and 32-channel torso-cardiac coil. The conventional WHC-MRA 3D bSSFP (conv-3DbSSFP) sequences were set to cover whole heart axial slab orientation using navigator and vector cardiac gating with the following parameters: FOV (mm) = 350×315, in-plane resolution (mm) = 1.39×1.39, slice thickness (mm) = 1.7mm/0.85mm overlap, TR/TE (ms) = 4.6/2.3, C-SENSE factor = 6.0, NSA = 1, scan time= 1:54~3:23 (depend on heart-beat, respiratory pattern and parameters). The parameters of zoomed WHC-MRA using 3D Vane/d-Vane without/with navigator gating were as follows: FOV (mm) = 200×200, radial percentage(%)=150,335 (335% was 3D d-Vane only setting), in-plane resolution (mm) = 1.39×1.39, slice thickness (mm) = 1.7mm/0.85mm overlap, TR/TE (ms) = 4.6/2.3, SENSE factor = 2, NSA = 1, scan time= 2:59~9:21 (depend on heart beat and slice direction coverage) and self-respiratory gating (SR-gating) was adopted only for 3D d-Vane. Images were assessed by using contrast to noise ratio (CNR); efficiency of CNR (CNReff). Signal intensity (SI) and standard deviation (SD) were measured at left ventricle myocardium (LVM), epicardial fat (LV-EF), and blood (LVB). CNReff was calculated as the ratio of CNR to the square root of scan time.Results & Discussion
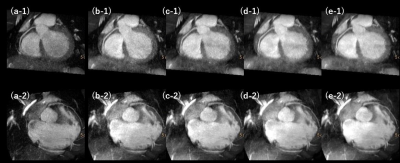
A significant difference of CNR in LVB/LV-EF was observed between 3D d-Vane and other methods at the radial percentage 335%. There was no significant difference between the CNR in LVB/LV-EF and LVB/LVM. However, when the time efficiency of 3D d-Vane at the radial percentage 150%/150% was used, the CNReff of 3D d-Vane became clearly higher than that of both 3D Vane and conv-3DbSSFP. The CNR (LVB/LV-EF or LVM) of the 3D d-Vane was largest at 335%, followed in order by 150%+SR-gating2.0, 150%+SR-gating1.5, and 150%. The CNReff was largest at 150%, followed in order by 150%+SR-gating1.5, 150%+SR-gating2.0, and 335%. The CNR of small FOV 3D d-Vane was comparable to that of the conventional sequence and 3D Vane. Moreover, it improved the CNReff compared to the conventional sequences and 3D Vane with shorter scan time and the same in-plane resolution. This was achieved because matrices can be reduced as well as FOV and the high-frequency component of k-space like a diamond shape. The 3D d-Vane with an averaging effect of central k-space of radial scan can adopt self-navigator and automatically correct the breath motion. This suggests that the 3D d-Vane may be able to reduce the respiratory motion artifact without using the respiratory navigator gating.Conclusion
In conclusion, small FOV WHC-MRA using 3D d-Vane can improve the image quality of WHC-MRA without extended scan time while maintaining the contrast and reducing the motion artifacts.Acknowledgements
No acknowledgement found.References
(1)Weber, Oliver M., Alastair J. Martin, and Charles B. Higgins. "Whole‐heart steady‐state free precession coronary artery magnetic resonance angiography." Magnetic resonance in medicine 50.6 (2003): 1223-1228.
(2) Block, Kai Tobias, et al. "Towards routine clinical use of radial stack-of-stars 3D gradient-echo sequences for reducing motion sensitivity." Journal of the Korean Society of Magnetic Resonance in Medicine 18.2 (2014): 87-106.
(3) Wundrak, Stefan, et al. "A small surrogate for the golden angle in time-resolved radial MRI based on generalized fibonacci sequences." IEEE transactions on medical imaging 34.6 (2015): 1262-1269.
(4)Zhou, Ziwu, et al. "Golden‐ratio rotated stack‐of‐stars acquisition for improved volumetric MRI." Magnetic Resonance in Medicine (2017).
(5) Yoshida T, et al. “Free-breathing zoomed whole heart coronary MRA without respiratory gating using small-FOV 3D stack-of-stars radial sequence with pseudo-golden angle sampling.” 45th JSMRM (2017):O2-41. 26th ISMRM (2018): 2997.
Figures