2781
Free-breathing MRCP using motion compensated 3D Cartesian turbo spin-echo imaging1Department of Radiotherapy, University Medical Center Utrecht, Utrecht, Netherlands, 2Computational Imaging Group for MRI diagnostics and therapy, Centre for Image Science, Utrecht, Netherlands, 3BIU MR, Philips Healthcare, Best, Netherlands, 4Department of Radiology, University Medical Center Utrecht, Utrecht, Netherlands
Synopsis
Magnetic resonance cholangiopancreatography (MRCP) is crucial for the diagnosis of biliary/pancreatic duct disease. However, conventional respiratory triggered (RT-MRCP) scans require long acquisition times and ultimately fail in patients with irregular breathing. In this work we propose a free-breathing motion corrected MRCP scan (MOCO-MRCP) based on a rewinded Cartesian Acquisition with Spiral Profile ordering (rCASPR). MOCO-MRCP eliminates idle time associated with respiratory triggering, thereby increasing the robustness to motion artefacts while reducing the overall scan time compared to RT-MRCP. We show preliminary results of MOCO-MRCP in three patients with suspected biliary/pancreatic duct disease.
Introduction
Magnetic resonance cholangiopancreatography (MRCP) is an important imaging modality for the diagnosis of biliary and pancreatic duct disease. Conventional MRCP sequences rely on heavily T2-weighted (echo time > 500 ms) 3D turbo spin-echo scans acquired with respiratory triggering (RT). The RT-MRCP leads to lengthy acquisitions that provide high image quality in some patients, but provide non-diagnostic results in patients with irregular breathing. As a consequence, recent works have focused on highly accelerated single breathhold MRCP scans using Compressed Sense (CS) to provide improved resilience to motion artefacts and to reduce scan time[1]. However, CS-MRCP requires long breathholds, which is not sustainable for some patients. In this work we propose a potential third flavour of MRCP scan, which is based on a free-breathing motion corrected MRCP scans, which we call (MOCO-MRCP). The key idea is to acquire data in free-breathing using a rewinded Cartesian Acquisition with SPiRal profile ordering (rCASPR)[2], which allows flexible contrast settings (long TE etc.) and self-navigated respiratory motion correction in the image reconstruction[3]. The rationale is that MOCO-MRCP eliminates idle time associated with respiratory triggering, thereby increasing the robustness to motion artefacts while reducing the overall scan time compared to RT-MRCP. In this work we investigate the technical feasibility of MOCO-MRCP in patients with suspected biliary/pancreatic duct disease.Methods
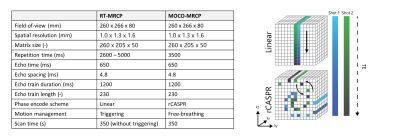
Image acquisitionFour patients with suspected biliary/pancreatic duct disease were scanned as part of a clinical exam on a 1.5T MR system (Philips Ingenia, Best, the Netherlands) with a 12 channel posterior and a 16 channel anterior receive coil. MR examination consisted of the conventional diagnostic protocol, including the RT-MRCP scan, with the addition of the MOCO-MRCP scan. The RT-MRCP was triggered with the respiratory belt. The total effective scan time and sequence parameters of RT-MRCP and MOCO-MRCP are the same, with detailed parameters shown in Fig.1-A. However, the total scan time of RT-MRCP was approximately 30 % longer due to the triggering. The only difference between the two MRCP scans is that MOCO-MRCP acquires the k-space data using the rCASPR phase encode scheme while the RT-MRCP uses the conventional linear (LIN) phase encode scheme (Fig-1B). The number of phase encodes of the rCASPR interleaves correspond exactly with the echo train length.
Image reconstruction
Prior to the TSE sequences a reference scan, implemented by the vendor, was acquired to generate the coil sensitivity maps[4]. K-space data were exported using Reconframe (Gyrotools, Zurich, CH) and were prewhitened and the multi-channel kx,y = (0, 0) projections were used to estimate the respiratory motion surrogate using the coil clustering method[5-6]. The motion surrogate was subsequently used to reorder the data across respiratory phases using soft-weighted amplitude binning. The resulting respiratory sorted k-space was downsampled to 4x4x4mm3 to reduce the undersampling artefacts[7] while maintaining sufficient resolution for motion estimation[8]. Respiratory correlated 4D-MRI images were reconstructed with a locally low rank-constrained methods[9] using the BART toolbox[10]. The 4D-MRI was subsequently registered to the exhale position using an edge based variational method for non-rigid registration (Evolution)[11]. The obtained motion fields were subsequently used for a motion compensated image reconstruction[12-13].
Image analyses
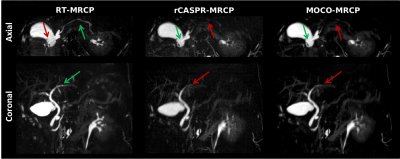
The rCASPR based MRCP scan was compared to the RT-MRCP in the following way: the rCASPR MRCP scan was reconstructed without motion correction (rCASPR-MRCP) and with motion correction (MOCO-MRCP) and compared to the RT-MRCP. The image comparison for now is completely qualitatively.
Results and Discussion
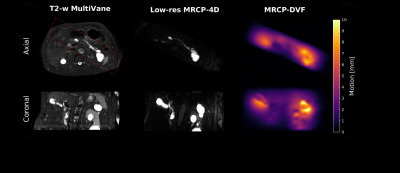
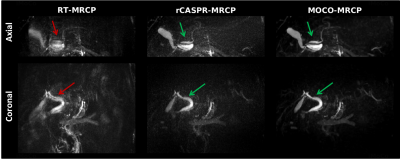
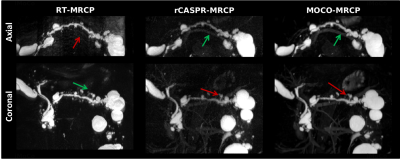
Figure 2 shows a representative result of a MRCP dataset, which shows a conventional T2-weighted MultiVane scan and the corresponding low resolution 4D-MRCP slice with the quantified motion fields. Note that the MRCP scans are planned in an oblique orientation (red box). Figure 3-5 show a side-by-side comparison of the maximum intensity projections of the RT-MRCP, rCASPR-MRCP and MOCO-MRCP. RT-MRCP shows considerable ghosting/motion related artefacts in patients where the respiratory triggering is difficult (Figure 3-4). These motion artefacts are already partially reduced using rCASPR-MRCP, which reflects the inherent motion robustness of the rCASPR trajectory. The inclusion of the motion compensation in the reconstruction results into an improved sharpness, indicating that the inclusion of the motion compensation in the reconstruction provides additional value. However, in a patient with very regular breathing the motion estimation could not capture the complete extent of the motion, which resulted in some additional blurring when compared to an RT-MRCP scan (Figure 5). The incomplete motion estimation could be related to intrashot motion, due to the relatively long shot duration (1200 ms). The inherent trade-off between the two methods is that RT-MRCP could provide sharper images at the cost of a considerably increased risk of motion artefacts. From a clinical perspective, the potential for slight blurring from MOCO-MRCP might be preferable over an increased risk for a non-diagnostic acquisition from RT-MRCP that requires the patient to be recalled.Conclusion and Future Work
This preliminary study has demonstrated the feasibility of performing free-breathing respiratory motion compensated MRCP with a 3D rCASPR turbo spin-echo acquisition in patients with biliary and pancreatic duct disease. rCASPR MOCO-MRCP provides a new flavour of MRCP with improved robustness to motion artefacts, potential to reduce the scan time and to increase the scanning comfort. Further clinical evaluation is required to assess the diagnostic performance of the proposed MOCO-MRCP sequence.Acknowledgements
This work is part of the research program HTSM with project number 15354, which is (partly) financed by the Netherlands Organization for Scientific Research (NWO) and Philips Healthcare.References
[1] Lohofer F K, Kaissis G A, Rasper M, Katemann C, Hock A, Peeters J M, Schlag C, Rummeny E J, Karampinos D and Braren R F; 2019; Magnetic resonance cholangiopancreatography at 3 Tesla: Image quality comparison between 3D compressed sensing and 2D single-shot acquisitions; European Journal of Radiology; 115(February), 53–58.
[2] Bruijnen T, Akdag O, Bruel C, Stemkens B, Schakel T, Lagendijk J, van
den Berg C and Tijssen RHN; 2020; Free-breathing 3D T2-weighted TSE using Cartesian acquisition with rewinded spiral profile ordering (rCASPR) for abdominal radiotherapy; in Proc. ISMRM 28.
[3] Cruz G, Atkinson D, Buerger C, Schaeffter T and Prieto C; 2016; Accelerated motion corrected threedimensional abdominal MRI using total variation regularized SENSE reconstruction; Magnetic Resonance in Medicine 75(4), 1484–1498.
[4] Pruessmann K P, Weiger M, Scheidegger M B and Boesiger P; 1999; SENSE: Sensitivity encoding forfast MRI; Magnetic Resonance in Medicine.
[5] Zhang T, Cheng J Y, Chen Y, Nishimura D G, Pauly J M and Vasanawala S S; 2016; Robust selfnavigated body MRI using dense coil arrays; Magnetic Resonance in Medicine; 76(1), 197–205.
[6] Feng L, Axel L, Chandarana H, Block K T, Sodickson D K and Otazo R; 2016; XD-GRASP: Golden-angle radial MRI with reconstruction of extra motion-state dimensions using compressed sensing; Magnetic Resonance in Medicine; 75(2), 775–788.
[7] Glitzner M, De Senneville B D, Lagendijk J J, Raaymakers B W and Crijns S P; 2015; On-line 3D motion estimation using low resolution MRI Physics in Medicine and Biology; 60(16); N301–N310.
[8] Zhu X, Chan M, Lustig M, Johnson K M and Larson P E; 2020; Iterative
motion-compensation reconstruction ultra-short TE (iMoCo UTE) for
high-resolution free-breathing pulmonary MRI; Magnetic Resonance in
Medicine 83(4), 1208–1221.
[9] Uecker M, Ong F, Tamir J I, Bahri D, Virtue P, Cheng J, Zhang T and Lustig M; 2015; BerkeleyAdvanced Reconstruction Tools; Proc. Intl. Soc. Mag. Reson. Med. 73(2), 828–842.
[10] Denis de Senneville B, Zachiu C, Ries M and Moonen C; 2016; EVolution: an edge-based variational method for non-rigid multi-modal image registration; Physics in medicine and biology; 61(20), 7377–7396.
[11] Batchelor P G, Atkinson D, Irarrazaval P, Hill D L G, Hajnal J and Larkman D; 2005; Matrix description of general motion correction applied to multishot images; Magnetic Resonance in Medicine 54(5), 1273–1280.
Figures