2780
3D breath-hold magnetic resonance cholangiography using compressed sensing acceleration in living donor liver transplantation donors1Tianjin First Central Hospital, Tianjin, China, 2MR Collaboration, Siemens Healthcare Ltd., Beijing, China, 3MR Application Development, Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
This study investigated the feasibility of optimized breath-hold compressed-sensing accelerated magnetic resonance cholangiography (BH-CS-MRCP) in visualizing the biliary system in living donor liver transplantation (LDLT) donors. Conventional navigator-triggered (NT) MRCP was performed preoperatively, and optimized BH-CS-MRCP was performed both preoperatively and one month after surgery. The optimized BH-CS-MRCP protocol showed similar motion or blurring artifacts, overall image quality, background suppression, and biliary duct depiction compared with conventional NT-MRCP protocols. This suggests that optimized BH-CS-MRCP with a short acquisition time (17 s) can be used for preoperative and postoperative evaluation of biliary ducts in LDLT donors.
Introduction and purpose
Three-dimensional (3D) navigator-triggered (NT) magnetic resonance cholangiography (MRCP) has been widely used for the preoperative evaluation of biliary tree anatomy in living donor liver transplantation (LDLT) donors [1]. Recently developed compressed-sensing (CS) accelerated MRCP has shown great potential in shortening the acquisition time, particularly for breath-bold (BH) examinations [2-4]. In addition, optimized BH-CS-MRCP with a smaller field-of-view (FOV), higher resolution, and increased acceleration factor showed better background signal suppression and visibility of intrahepatic bile ducts [4]. In LDLT donors, the biliary tree is non-dilated, which increases the difficulty of imaging. A previous study focused on qualitative image analysis and demonstrated the feasibility of BH-CS-MRCP used in LDLT donors [5]. In our study, we used an optimized BH-CS-MRCP with a smaller FOV, higher resolution, and increased acceleration factor and compared this with conventional NT-MRCP, both qualitatively and quantitatively. The purpose of this study was to evaluate the clinical feasibility of an optimized BH-CS-MRCP in visualizing the biliary system in LDLT donors.Methods
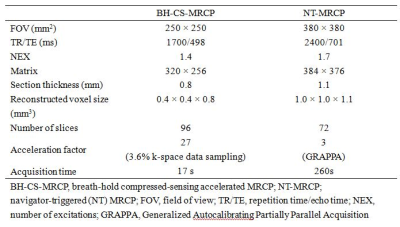
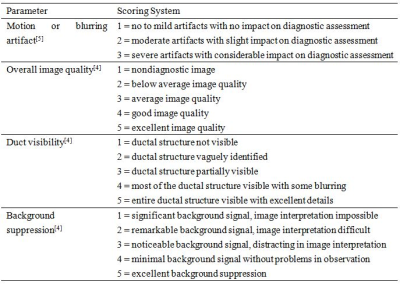
The institutional review board approved this prospective study, and all patients provided written informed consent. Sixteen donors (12 men and 4 women, median age, 32 years; age range, 23-56 years) who underwent LDLT were consecutively enrolled. Two 3D MRCP protocols (conventional NT-MRCP and optimized BH-CS-MRCP) were performed preoperatively in random order, and the BH-CS-MRCP protocol was also performed one month after the surgeries on a 3T MR system (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany). CS-measurements were performed using a prototype 3D SPACE sequence. Scanning parameters are shown in Table 1. The qualitative image quality evaluation, including motion or blurring artifact, overall image quality, duct visibility (common bile duct, CBD; common hepatic duct, CHD; cystic duct, CD; left hepatic duct, LHD; right hepatic duct, RHD; right anterior hepatic duct, RAHD; and right posterior hepatic duct, RPHD) and anatomy variations of the biliary tree were independently evaluated by two radiologists, who were blinded to the protocols. The scoring system is shown in Table 2 [4-5]. The quantitative image quality evaluation, including signal-to-noise ratio (SNR) of the CBD, contrast ratio between the CBD and periductal tissue (CR), and contrast-to-noise ratio (CNR) of the CBD and liver parenchyma, were also measured and calculated [4]. Diagnostic accuracy of anatomy variations of the biliary tree was assessed using intraoperative cholangiography and surgical records as a reference standard. The quantitative and qualitative image quality parameters were compared between different scanning protocols preoperatively and compared pre- and postoperatively.Results
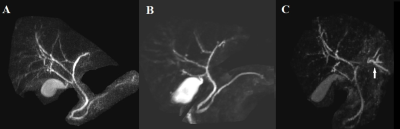
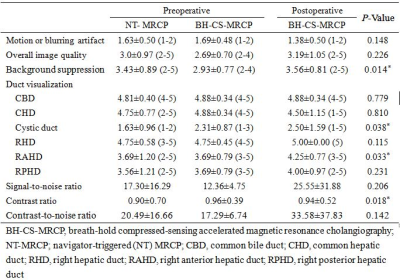
Interobserver agreement of the qualitative evaluation ranged from good to excellent (K = 0.712 – 1), and quantitative evaluation was good (ICC = 0.801 - 0.934). In the preoperative evaluation, type I bile duct anatomy was identified in 15 donors, and six candidates presented with other variation types (type II in two donors, type III in three donors, and type IV in one donor), and both protocols depicted the anatomy variations exactly (Figure 1). Optimized BH-CS-MRCP showed similar motion or blurring artifacts and overall image quality compared with conventional NT-MRCP (all P>0.05). The preoperative optimized BH-CS-MRCP showed worse background suppression compared with conventional NT-MRCP, but postoperative optimized BH-CS-MRCP showed similar background suppression compared with conventional NT-MRCP. The visibility of CBD, CHD, CD, LHD, RHD, and RPHD was similar between the two MRCP protocols (all P >0.05). Optimized BH-CS-MRCP showed a better depiction of the cystic duct and RAHD. The SNR of CBD and CNR of the CBD and liver were comparable between both MRCP protocols (all P >0.05), and optimized BH-CS-MRCP showed better CR between the CBD and periductal tissue (P=0.018) (Table 3).Discussion and Conclusions
Optimized BH-CS-MRCP showed comparable image quality to conventional NT-MRCP in visualizing the biliary system in LDLT donors and can be used for preoperative and postoperative evaluation of biliary ducts, with a short acquisition time (17 s).Acknowledgements
This work was supported by the National Natural Science Foundation for Young Scientists of China (81901710).References
1. Hyodo T, Kumano S, Kushihata F, et al. CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol. 2012 Jul;85(1015):887-896.
2. Chandarana H, Doshi AM, Shanbhogue A, et al. Three-dimensional MR Cholangiopancreatography in a Breath Hold with Sparsity-based Reconstruction of Highly Undersampled Data. Radiology. 2016;280(2):585-594.
3. Zhu L, Wu X, Sun Z, et al. Compressed-Sensing Accelerated 3-Dimensional Magnetic Resonance Cholangiopancreatography: Application in Suspected Pancreatic Diseases. Invest Radiol. 2018;53(3):150-157
4. Song JS, Kim SH, Kuehn B, et al. Optimized Breath-Hold Compressed-Sensing 3D MR Cholangiopancreatography at 3T: Image Quality Analysis and Clinical Feasibility Assessment. Diagnostics (Basel). 2020;10(6):376.
5. Ono A, Arizono S, Kohno S, et al. Diagnostic accuracy of 3D breath-hold MR cholangiography using compressed sensing acceleration in visualizing non-dilated biliary system in living donor liver transplantation donors. Acta Radiol. 2019;60(10):1209-1215.
Figures