2772
Assessment of hepatic signal change in free breathing continuous multiphasic dynamic EOB-MRI with compressed sensing and self-gating technique
Masaya Tanabe1, Masahiro Tanabe1, and Katsuyoshi Ito1
1Yamaguchi University, Ube City, Japan
1Yamaguchi University, Ube City, Japan
Synopsis
In the analysis of the hepatic contrast enhancement parameters based on continuous data of the signal changes over time obtained by free-breathing continuous multiphasic dynamic EOB-MR imaging using compressed sensing and self-gating technique, contrast enhancement ratio (CER) in the portal phase and 5min early hepatocyte phase had significant correlation with hepatic contrast enhancement effects in the 20min hepatobiliary phases and showed significant difference between sufficient and insufficient hepatobiliary phases enhancement groups, suggesting that sufficient 20min hepatobiliary phases enhancement may be estimated by the CER in the portal phase and 5min early hepatocyte phase.
INTRODUCTION:
In liver MR
imaging using gadoxetic acid disodium (Gd-EOB-DTPA), multiphasic dynamic
imaging including arterial, portal, transitional and hepatobiliary phases
during a separate breath-holding has been widely used to detect and
characterize hepatic lesions. Additionally, some studies showed that the signal
intensity (SI) of the hepatic parenchyma in the hepatobiliary phase (HBP) was
related to the severity of hepatic fibrosis and could be used to estimate the
liver function. The recent introduction of compressed sensing (CS) combined
with a self-gating technique enables continuous multiphasic dynamic MR imaging
during free-breathing for several minutes, allowing for the evaluation of the
continuous signal change of the hepatic parenchyma over time. However, there
have been no studies evaluating the relationship between the continuous signal
change of the liver and the hepatic contrast enhancement effect in the HBP. The
purpose of this study was to investigate the relationship between the hepatic
contrast enhancement effect in the HBP and the hepatic contrast enhancement parameters
based on data of continuous signal changes obtained by free-breathing continuous
multiphasic dynamic EOB-MR imaging using CS and self-gating technique.
METHODS:
Our study included
96 patients who underwent free-breathing continuous multiphasic dynamic EOB-MR
imaging of the liver using CS and self-gating technique due to HCC, hemangioma,
or liver metastases. Free-breathing continuous dynamic T1-weighted images were obtained
every 11 seconds for about 5 minutes including 1 precontrast and 28
post-contrast phases. The injection of contrast materials was started just
after the completion of the precontrast phase acquisition. Finally, HBP images
were obtained 20 min. after the contrast injection as 30th phase images. The
region of intensity (ROI) was set as large as possible at two locations in the
right lobe and one in the left lobe, avoiding blood vessels, and the SI of each
temporal phase was measured at the same location. The average of the SI of the
three ROIs was taken as the signal intensity for each time phase. Several contrast
enhancement parameters based on data of continuous signal changes were
calculated to evaluate the enhancement effects of the liver parenchyma. The contrast
enhancement ratio (CER) from phase X to phase y was calculated as follows: CERy-x:
(SIy -SIx)/SIx. The gradient of the regression
line was also calculated if necessary. We have calculated CER4-pre
(arterial enhancement rate), CER7-5 (portal-arterial enhancement
rate), CER7-pre (portal enhancement rate), CER28-pre (5min
early hepatocyte enhancement rate), CER28-7 (early hepatocyte-portal
enhancement rate), and CERHBP-pre (20min hepatocyte enhancement
rate). For the gradient of a regression line (Gradienty-x : the
gradient from the phase X to the phase Y), we calculated Gradient4-2
(arterial transit gradient), Gradient7-4 (portal transit gradient),
Gradient7-2 (arterioportal transit gradient), Gradient28-7
(early hepatocytic transit gradient). According to the severity of liver
fibrosis (F0-F2, F3-F4), patients can be divided into two groups with
sufficient or insufficient liver enhancement based on CERHBP-pre with
a cutoff value of 0.7031. Then,
each parameter was compared between these two groups. In addition, age, gender,
total bilirubin, prothrombin time, albumin, and eGFR were also compared between
the two groups (Wilcoxon's rank sum test). A nonparametric test was also
performed to determine the effect of each item on the SI of the HBP (Spearman's
rank sum correlation coefficient).
RESULTS:
In the analysis of
the arterioportal phases (phases 1-7), CER7-pre in the sufficient
HBP enhancement group was significantly higher than that in the insufficient
HBP enhancement group (0.50 vs 0.44, p<0.001) while the differences in CER4-pre,
Gradient4-2, Gradient7-4 and Gradient7-2 were
not significant between the two groups. Regarding 5min early hepatocyte phase
(phases 1-28) analysis, significant differences were observed in CER28-pre,
CER28-7 and Gradient28-7 between the two groups (0.64 vs
0.47, 0.10 vs 0.03, 1.27 vs 0.27, all p<0.001). The parameters of blood
sampling (total bilirubin, prothrombin time, albumin, and eGFR) showed
significant differences between the two groups (p=0.049~0.004). For the
strength of correlation between hepatic contrast enhancement effect in the 20min
HBP and each parameter, CER7-pre, CER28-pre, CER28-7,
and Gradient28-7 had higher correlation coefficients, compared with
total bilirubin, prothrombin time, albumin, and eGFR. CER28-pre
showed the highest correlation coefficient (0.838). (Table 1-3).
DISCUSSION:
Our study showed
that CER7-pre, CER28-pre and CER28-7 were
significantly well correlated with hepatic contrast enhancement effect in the
20min HBP, compared with the blood sampling parameters. In addition, CER7-pre,
CER28-pre and CER28-7 were significantly higher in the
sufficient HBP enhancement group than in the insufficient HBP enhancement
group. These facts suggested that the CER in the portal phase and 5min early hepatocyte
phase (CER7-pre, CER28-pre and CER28-7) may
help estimate the sufficient 20min HBP enhancement, and that these parameters
may be used to shorten the timing of imaging the HBP.
CONCLUSION:
In the analysis of
the hepatic contrast enhancement parameters based on continuous data of the
signal changes over time obtained by free-breathing continuous multiphasic
dynamic EOB-MR imaging using CS and self-gating technique, CER in the portal
phase and 5min early hepatocyte phase had significant correlation with hepatic
contrast enhancement effects in the 20min HBP, and showed significant
difference between sufficient and insufficient HBP enhancement groups,
suggesting that sufficient 20min HBP enhancement may be estimated by the CER in
the portal phase and 5min early hepatocyte phase.
Acknowledgements
No acknowledgement found.References
REFERENCES: References should use the suggested style below. 1. C Besa , M Wagner, et al. Detection of Liver Fibrosis Using Qualitative and Quantitative MR Elastography Compared to Liver Surface Nodularity Measurement, Gadoxetic Acid Uptake, and Serum Markers. J Magn Reson Imaging. 2018; 47: 1552-1561Figures
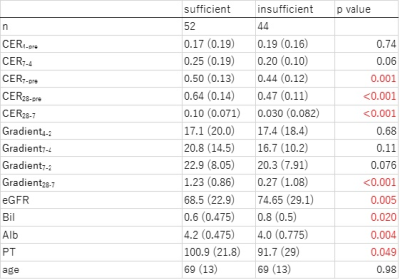
Comparison between sufficient HBP enhancement group (CERHBP-pre > or = 0.703) and insufficient HBP enhancement group (CERHBP-pre < 0.703) in each item. The median and interquartile range and p-value for each item are shown.
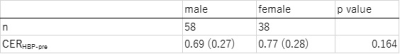
The result of the difference in CERHBP-pre between genders. The median and interquartile range and p-value are shown.
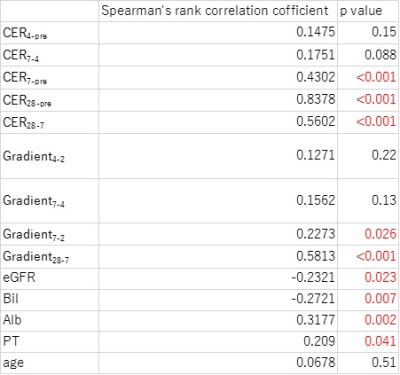
The results of the correlation between the SI of hepatic parenchyma in the HBP and each items. Spearman's rank sum correlation coefficient and p-value are shown.
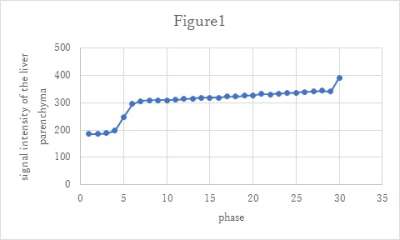
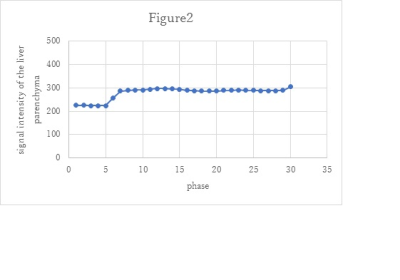
Signal-intensity changes of the liver parenchyma during free-breathing continuous multiphasic dynamic EOB-MR imaging using CS and self-gating technique in the case with sufficient hepatic parenchyma enhancement in the HBP; CERHBP-pre: 1.10, CER7-pre: 0.66.
Signal-intensity changes of the liver parenchyma during free-breathing continuous multiphasic dynamic EOB-MR imaging using CS and self-gating technique in the case with insufficient hepatic parenchyma enhancement in the HBP; CERHBP-pre: 0.35, CER7-pre: 0.28.