2579
DTI and NODDI assessment of posterior optic pathway function in sellar and parasellar tumor patients1Department of Electrical and Computer Engineering, Seoul National University, Seoul, Korea, Republic of, 2Department of Radiology, Seoul National University Hospital, Seoul, Korea, Republic of, 3Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea, Republic of
Synopsis
We investigated the impairment in the optic radiations affected by the anterior visual pathway compression using the diffusion tensor imaging (DTI), and neurite orientation dispersion and density imaging (NODDI). The results were correlated with the visual field impairment score (VFIS), which assesses the function of posterior visual pathway. The DTI and NODDI parameters in the optic radiations were significantly correlated with postoperative visual field improvement as well as preoperative visual field impairment in patients with the compression of optic chiasm. The study demonstrated the anterior visual pathway compression influences the visual field defect of the posterior visual pathway.
Introduction
In patients with sellar and parasellar tumors, it is crucial to evaluate the visual field impairment in the preoperative stage and to predict visual field improvement after surgery. The diffusion tensor imaging (DTI) provides fractional anisotropy (FA), mean diffusivity (MD), axial diffusivity (AD), and radial diffusivity (RD)1. Neurite orientation dispersion and density imaging (NODDI) provides intracellular volume fraction (Vic), the orientation dispersion index (ODI), and isotropic volume fraction (Viso)2. In a few DTI studies have reported the anterograde trans-synaptic degeneration from disruptions in visual input affected by compression of the optic chiasm3. In the study, FA in the optic radiation was shown to be significantly associated with visual impairment in patients with optic pathway glioma4-5 and reported reduced retinal nerve fibre layer thickness5. In this work, we investigated whether DTI and NODDI parameters in the optic radiations were associated with visual field impairments in the preoperative stage and visual field improvement after surgery.Methods
Eighty-one participants (40 males and 41 females; mean age of 48.8 ± 15.4 years) with sellar and parasellar tumors were included in the study. MRI scanning and ophthalmologic examination were performed before and after tumor resection. A visual field impairment score (VFIS), a quantitative scoring system for visual field defect, was assessed the visual field defect reflecting the function of each optic tract based on the results of the Goldmann or Humphrey perimetry. The VFIS ranged 0 (normal visual field) to 8 (all parts of the unilateral optic tract had visual impairment). If the right score is 4, it indicates 4 of 8 defects in the left visual field which corresponds to the function of the right optic radiation. Since each unilateral optic radiation within a participant was analysed separately, our study included a total of 162 optic radiations from 81 participants.The multi-shell diffusion weighted imaging using 2D echo planar imaging for both DTI and NODDI processing was acquired at Siemens 3T Skyra scanner with TR/TE=3000/105 ms, FOV=240×240 mm2, voxel size=1.5×1.5 mm2, slice thickness=4 mm, b = 300 s/mm2 with 9 diffusion directions, b = 700 s/mm2 with 36 directions, b = 2000 s/mm2 with 72 directions. The two opposite phase encoding directions scan with b = 0 s/mm2 was acquired.
DTI processing was performed by FMRIB software library (FSL) version 5.0.8 and NODDI parameters were processed using accelerated microstructure imaging via convex optimization. The preoperative and postoperative images within each participant were linearly registered using FSL.
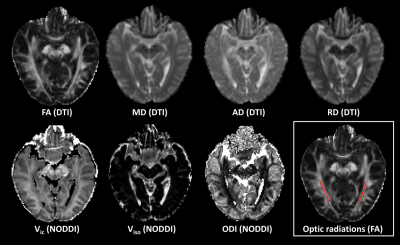
High intensity regions of optic radiations in one slice of FA map were manually drawn using MITK workbench (Figure 1). The statistical analysis was performed with SPSS 25.0. The comparison between preoperative and postoperative results using paired t-test, partial correlation between preoperative imaging parameters and VFIS, and ordinal logistic regression for degree of postoperative improvement were performed. The age, tumor height, and symptom duration were adjusted in analyses. P-value of < 0.05 was considered as statistically significant.
Results
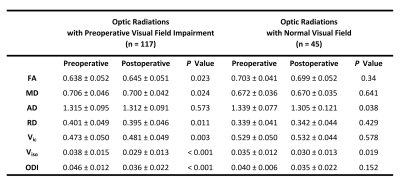
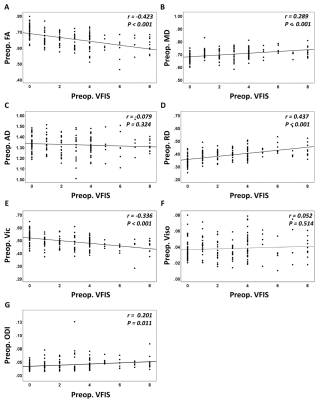
The results of comparison between preoperative and postoperative data in optic radiations with preoperative visual field impairment (n = 117) and optic radiations with normal visual fields (n = 45) are shown in figure 2. In the optic radiations with visual field impairment, the FA (p = 0.023) and Vic (p = 0.003) significantly increased, while the MD (p = 0.024) and RD (p = 0.011) values significantly decreased after surgery (p < 0.001 for ODI and Viso). However, in the optic radiations with normal visual fields, only AD and Viso, significantly change after surgery (p > 0.05).The preoperative VFIS had significant negative correlations with preoperative FA (r = -0.423, p < 0.001) and Vic (r = -0.336, p < 0.001), and significant positive correlations with MD (r = 0.289, p < 0.001), RD (r = 0.437, p < 0.001), and ODI (r = 0.201, p = 0.011) (Figure 3).
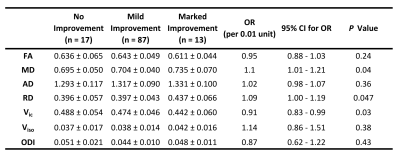
The degree of ΔVFIS, which represented changes in visual fields after surgery, for 117 optic radiations with preoperative visual field impairment was as follows: n = 17 with no improvement or worse after surgery, n = 87 with mild improvement, and n = 13 with marked improvement. As a result, preoperative lower Vic (Odds ratio (OR) = 0.91, 95% confidence interval (CI), 0.83 - 0.99, p = 0.03) and higher MD (OR = 1.1, 95% CI, 1.01 - 1.21, p = 0.04) and RD (OR = 1.09, 95% CI, 1.00 - 1.19, p = 0.047) were significantly associated with ΔVFIS (Figure 4).
Discussion
Several preoperative DTI and NODDI parameters in the optic radiations were significantly correlated with the preoperative VFIS and postoperative ΔVFIS. We presume that anterior visual pathway compression might cause decreased neurite density and demyelination in the optic radiation. Our results were similar to a few previous studies that reported trans-synaptic degeneration in sellar or parasellar lesions5-6. Changes of DTI and NODDI parameters in the optic radiation may reflect trans-synaptic degeneration.Conclusion
In summary, we demonstrated that DTI and NODDI parameters in the optic radiations were associated with postoperative improvement as well as preoperative visual field impairments. It may help in predicting visual field improvement after surgery in patients with sellar or parasellar tumors.Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT & Future Planning (2017R1A2B2008412) and MSIT (NRF-2018R1A4A1025891).References
1. Basser PJ, Mattiello J, LeBihan D. MR diffusion tensor spectroscopy and imaging. Biophys J. 1994;66(1):259-67.
2. Zhang H, Schneider T, Wheeler-Kingshott CA, Alexander DC. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage. 2012;61(4):1000-16.
3. Gabilondo I, Martínez‐Lapiscina EH, Martínez‐Heras E, Fraga‐Pumar E, Llufriu S, Ortiz S, Bullich S, Sepulveda M, Falcon C, Berenguer J. Trans‐synaptic axonal degeneration in the visual pathway in multiple sclerosis. Ann Neurol. 2014;75(1):98-107.
4. de Blank PMK, Berman JI, Liu GT, Roberts TPL, Fisher MJ. Fractional anisotropy of the optic radiations is associated with visual acuity loss in optic pathway gliomas of neurofibromatosis type 1. Neuro Oncol. 2013;15(8):1088-95.
5. Phal PM, Steward C, Nichols AD, Kokkinos C, Desmond PM, Danesh-Meyer H, Sufaro YZ, Kaye AH, Moffat BA. Assessment of optic pathway structure and function in patients with compression of the optic chiasm: a correlation with optical coherence tomography. Invest Ophthalmol Vis Sci. 2016;57(8):3884-90.
6. Rutland JW, Padormo F, Yim CK, Yao A, Arrighi-Allisan A, Huang K-H, Lin H-M, Chelnis J, Delman BN, Shrivastava RK. Quantitative assessment of secondary white matter injury in the visual pathway by pituitary adenomas: a multimodal study at 7-Tesla MRI. J Neurosurg. 2019;1(aop):1-10.
Figures