2577
The Added Value of Inflow-Based Vascular-Space-Occupancy and Diffusion-Weighted Imaging in Preoperative Grading of Gliomas1Department of Medical Imaging, Nanfang Hospital, Southern Medical University, Guangzhou, China, 2Neurosection, Division of MRI Research, Department of Radiology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 3F.M. Kirby Research Center for Functional Brain Imaging, Kennedy Krieger Institute, Department of Radiology, Johns Hopkins University School of Medicine, Baltimore, MD, United States, 4Department of Neurosurgery, Nanfang Hospital, Southern Medical University, Guangzhou, China
Synopsis
Glioma grading is vital for planning therapeutic approaches and assessing prognosis and response to treatment. Advanced MR imaging provides physiological information of brain tumors in microcirculation, cell and molecular levels, thus improving the preoperative prediction of glioma grade. In this study, we studied the value of combined inflow-based vascular-space-occupancy (iVASO) MR imaging and diffusion-weighted imaging (DWI) in preoperative prediction of gliomas grade. The results showed that combined iVASO and DWI improved the diagnostic performance of glioma grading. This suggests that the combined application of iVASO and DWI might be used as part of the routine brain tumor imaging protocol.
INTRODUCTION
Accurate prediction of gliomas grade preoperatively is clinically desired1,2. Structural MR imaging does not allow for accurate predicting grade of gliomas. Diffusion-weighted imaging (DWI) can quantify tumor cellularity in vivo and distinguish high- and low-grade glioma effectively. Perfusion-weighted imaging (PWI) provides information about angiogenesis and vascularity. Inflow-based vascular-space-occupancy (iVASO) is a novel perfusion technique without the need for exogenous contrast agents. The present study aimed to study whether combined inflow-based vascular-space-occupancy (iVASO) MR imaging and diffusion-weighted imaging (DWI) improve the diagnostic accuracy in the preoperative grading of gliomas.METHODS
Fifty-one patients with histopathologically confirmed diffuse gliomas underwent preoperative structural MR imaging, iVASO and DWI (Achieva, TX, Philips). We performed 2 qualitative consensus reviews: 1) structural MR images alone and 2) structural MR images with iVASO and DWI. Relative arteriolar cerebral blood volume (rCBVa) and minimum ADC (mADC) were compared between low-grade and high-grade gliomas. Receiver operating characteristic (ROC) analysis was performed to compare tumor grading efficiency of rCBVa, mADC and the combination of the two parameters.RESULTS
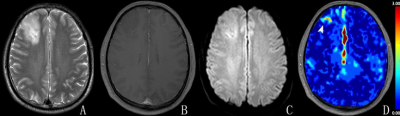
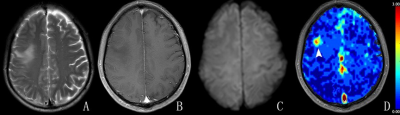
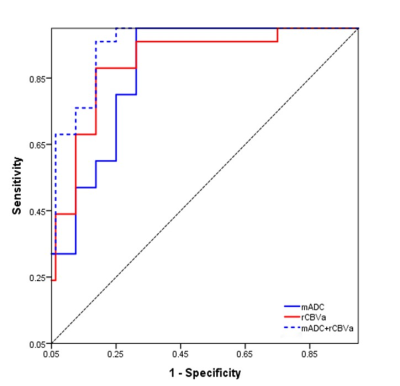
Two observers diagnosed accurate tumor grade in 40 of 51 (78.4%) patients in the first review (Table 1) and in 46 of 51 (90.2%) in the second review (Figures 1 and 2). Both rCBVa and mADC showed significant differences between low-grade and high-grade gliomas. ROC analysis (Table 2) gave a threshold value of 1.52 for rCBVa and 0.85×10-3 mm2/s for mADC to provide a sensitivity and specificity of 88.0 and 81.2% and 100.0 and 68.7%, respectively. The area under the ROC curve was 0.87 and 0.85 for rCBVa and mADC, respectively (Figure 3). The combination of rCBV and mADC values increased the area under the ROC curve to 0.92.DISCUSSION
In our study, we could use iVASO-rCBVa and minADC for preoperative grading of gliomas. Furthermore, we found an adjunctive value of iVASO and ADC maps in the glioma grading compared with structural images alone. Endothelial neovascularization is an important histopathologic feature that reflects glioma malignancy3 and increased vascularity is typically associated with higher tumor grade and aggressiveness4-8. iVASO, leveraging proton spins in the water molecules in blood as endogenous contrast agents, can quantify the arterial compartment of the microcirculation9. The present study demonstrated that iVASO-rCBVa can accurately distinguish low-grade and high-grade gliomas with the threshold value of 1.52. In general, glioma cell proliferation and cell density increase with WHO tumor grade3. High-grade gliomas tend to show a decreased diffusion rate of extracellular water molecules and a lower ADC5,7. In our present study, minimum ADC (mADC) values were significantly different between low-grade and high-grade gliomas. It was reported that the combination of different advanced MRI techniques could improve the diagnostic efficacy of glioma grading10,11. Our study showed that combining PWI and DWI improved the diagnostic efficacy of glioma grading. This was because combining structural and advanced MRI can provide us quantitative information on the biological characteristics of tumors in addition to accurate anatomical localization. Our study showed an increase of diagnostic accuracy of glioma grading (from 78.4% to 90.2%), through combination of structural MRI, iVASO and DWI images.CONCLUSION
iVASO and DWI showed added value in preoperative grading of glioma to structural MRI. The combined application of iVASO and DWI might be used as part of the routine brain tumor imaging protocol.Acknowledgements
No acknowledgement found.References
1. Rollin N, Guyotat J, Streichenberger N, et al. Clinical relevance of diffusion and perfusion magnetic resonance imaging in assessing intra-axial brain tumors. NEURORADIOLOGY. 2006;48(3):150-159.
2. Lee EJ, Lee SK, Agid R, et al. Preoperative grading of presumptive low-grade astrocytomas on MR imaging: diagnostic value of minimum apparent diffusion coefficient. Am J Neuroradiol. 2008;29(10):1872-1877.
3. Wesseling P, Capper D. WHO 2016 classification of gliomas. Neuropathol Appl Neurobiol. 2018;44(2):139-150.
4. Hirai T, Murakami R, Nakamura H, et al. Prognostic value of perfusion MR imaging of high-grade astrocytomas: long-term follow-up study. Am J Neuroradiol. 2008;29(8):1505-1510.
5. Sadeghi N, D'Haene N, Decaestecker C, et al. Apparent diffusion coefficient and cerebral blood volume in brain gliomas: relation to tumor cell density and tumor microvessel density based on stereotactic biopsies. Am J Neuroradiol. 2008;29(3):476-482.
6. Cao M, Suo S, Han X, et al. Application of a simplified method for estimating perfusion derived from diffusion-weighted MR imaging in glioma grading. FRONT AGING NEUROSCI. 2017;9:432.
7. Cha S. Update on brain tumor imaging: from anatomy to physiology. Am J Neuroradiol. 2006;27(3):475-487.
8. Maia AJ, Malheiros SM, Da RA, et al. MR cerebral blood volume maps correlated with vascular endothelial growth factor expression and tumor grade in non-enhancing gliomas. Am J Neuroradiol. 2005;26(4):777-783.
9. Brendle C, Hempel JM, Schittenhelm J, et al. Glioma grading and determination of IDH mutation status and ATRX loss by DCE and ASL perfusion. CLIN NEURORADIOL. 2018;28(3):421-428.
10. Kim HS, Kim SY. A prospective study on the added value of pulsed arterial spin-labeling and apparent diffusion coefficients in the grading of gliomas. AM J NEURORADIOL. 2007;28(9):1693-1699.
11. Hilario A, Ramos A, Perez-Nuñez A, et al. The added value of apparent diffusion coefficient to cerebral blood volume in the preoperative grading of diffuse gliomas. AM J NEURORADIOL. 2012;33(4):701-707.
Figures