2371
Reduced cerebrovascular reactivity and cerebral blood flow in White Matter Hyperintensities (WMHs)1Department of Radiology, Center for Biomedical Imaging, NYU Grossman School of Medicine, New York, NY, United States, 2Vilcek Institute of Graduate Biomedical Sciences, NYU Grossman School of Medicine, New York, NY, United States, 3Department of Radiology and Radiological Science, Johns Hopkins University, Baltimore, MD, United States, 4Department of Neurology, NYU Grossman School of Medicine, New York City, NY, United States
Synopsis
Understanding of in vivo vascular pathophysiology in white matter hyperintensities (WMHs) is still incomplete. Compared to grey matter, white matter is considerably less vascularized and tends to have lower blood flow. Therefore, sensitive detection and accurate estimation for white matter hemodynamics is crucial for early prevention and mechanistic understanding of WMHs pathogenesis and progression. In this study, we implemented advanced neurovascular MRI techniques to evaluate the white matter hemodynamics including cerebral blood flow and cerebrovascular reactivity in patients with varying degrees of WMHs.
Introduction
Small vessel disease (SVD) is a cerebral microvascular disorder in elderly populations that is highly associated with stroke and vascular dementia1-3. White matter hyperintensities (WMHs), which is common findings on brain T2-weighted MRI, are considered to be pathogenically associated with SVD4. Currently, although chronic hypoperfusion is deemed as the key pathogenic mechanism for WMHs progression, the causal relationship of CBF and WMHs needs additional evaluation5. It is technically challenging to obtain accurate vascular parametric estimation from small vessels in the white matter, which is considerably less vascularized compared to grey matter. Moreover, the autoregulation mechanism of the brain, which tends to compensate and maintain blood flow at constant level in ischemic regions, hampers the sensitive detection of CBF at early stage of SVD6. Therefore, in addition to CBF assessed in patients with WMHs in this study, we will evaluate cerebrovascular reactivity (CVR), another crucial vascular function that is less studied in white matter small vessels7. CVR is usually coupled with CBF alterations, denoting the vasodilatory capacity of modulating blood flow when demands of CBF increases.Methods
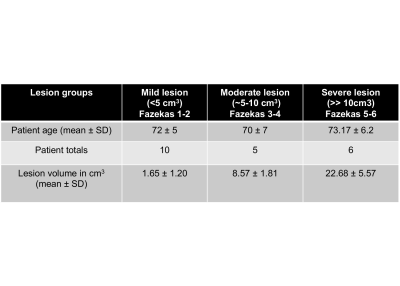
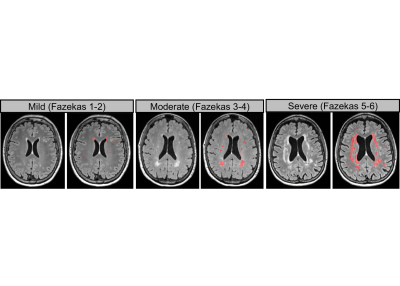
In this ongoing cohort, a total of 21 subjects were recruited for MRI scans with the following protocol. 1) 3D T2-FLAIR; 2) 3D T1-MPRAGE 3) 3D pseudo-continuous ASL (pCASL) (field-of-view: 220×220x144 mm3, voxel size: 3.4×3.4×4mm3, labeling duration: 1800 ms, PLD: 2000ms, TR/TE= 4120/12.56ms) along with a M0 scan (TE=10000ms); and 4) Gas-enhanced CVR-BOLD MRI (single-shot gradient-echo EPI, TR/TE=1500/21ms, field-of-view: 220×220x130mm3, voxel size 3.4×3.4×3.8mm3). WMHs lesions were semi-automatically segmented using FireVoxel software based on FLAIR images8 and sub-group into mild, moderate and severe group based on the total lesion volume and Fazekas score9 (in Table 1). WM mask was segmented using MPRAGE image by a multi-atals based segmentation method10. CBF was quantified based on ASL kinetics modeling (Blood T1: 1650ms, brain/blood partition coeff: 0.9 ml/g, labeling efficiency 0.85) at voxel-by-voxel basis for CBF map. Relative CBF (rCBF) was calculated as the ratio to whole brain average CBF. CVR was measured in assistance of a gas delivery systems that requires the patient inhale 5% CO2 during a 7-minute BOLD scan through mouth piece11. End-tidal CO2 (Et-CO2) trace was monitored by capnography device outside scanner room. BOLD time course and Et-CO2 time course are processed by multiple linear regression to find the minimum residual of fitting coefficient representing CVR index. The process was conducted on a voxel-by-voxel basis to generate CVR parametric map. rCBF and CVR map was registered to FLAIR images and T1-MPRAGE using SPM12 to obtain region-specific value for further evaluation of hemodynamic profile in WMHs patients. Statistical analysis: Student’s T test was used to examine the group-wise difference of CBF and CVR in mild, moderate and severe lesion groups. Pearson correlation was performed to examine the association of relative CBF and CVR with WMHs lesion volume.Results
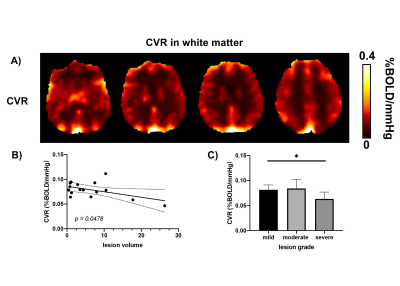
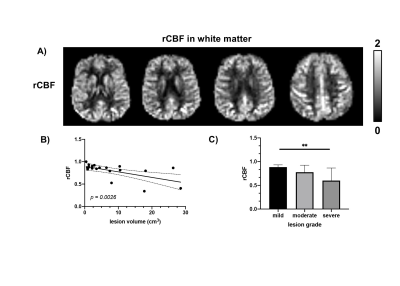
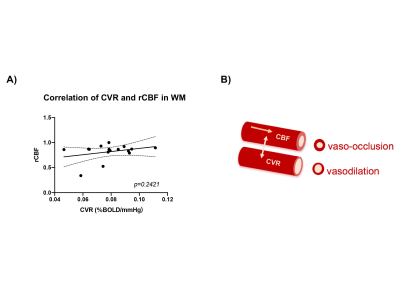
Figure 1 illustrates the representative T2-FLAIR images and their corresponding semi-automated segmentation results of WMHs in mild, moderate, and severe groups. In figure 2a), the representative CVR maps have been demonstrated. Figure 2b) shows the correlative analysis between white matter CVR and lesion volume, indicating that impaired CVR function could be associated with higher WMHs lesion loads. In figure 2C), group-wise analysis further revealed a significant difference (p=0.018) in white matter CVR between mild lesion and severe lesion. In Figure 3, the representative rCBF map has been illustrated as the same slice position with CVR map and correlation between lesion volume and rCBF in white matter indicates the potential hypoperfusion in white matter of WMHs patients. In addition, group-wise analysis suggested a significant difference (p=0.002) in rCBF between mild and severe lesion group. In figure 4, correlation analysis between rCBF and CVR in white matter indicated the potential correlation between CBF and CVR in various degree of WMHs lesions.Discussion
Based on the limited subject number of ongoing cohort, we observe a potential reduced CBF and CVR in WMHs patients with higher lesion loads. In the CBF data analysis, rCBF is the CBF with respect to the whole brain, which would correct the difference caused by individual variation of the global blood supply. Reduced rCBF has been observed in the patients with higher lesion loads, consistent with the hypothesis that hypoperfusion is one of the complications in WMHs. In CVR analysis, lower CVR has been observed with higher lesion loads, suggesting the potential impaired vasomotor function in white matter. The correlation analysis between rCBF and CVR reveals the potential coupled dysfunctions in white matter small vessels and their coupled effect is illustrated in Figure 4B).Conclusion
In this ongoing study, we investigated the white matter hemodynamic profile (CBF and CVR) in WMHs patients. Both microvascular functions in WM showed lower value in patients with higher WMHs lesion load and the rCBF and CVR measurements are potentially correlated. This paired CBF and CVR estimation could bring additional evaluation for microvascular integrity in white matter, elucidating the potential alternative mechanism of WMHs progression. Potential limitations of this study is that WM mask could introduce partial volume and the current limited sample size for analysis. In the future, more subjects need to be included for validation for this phenomenon.Acknowledgements
This study was funded by National Institute of Health grants (RF1 NS11041, R56 AG060822, R01 NS108491, R13 AG067684). This study is also supported by Alzheimer’s Association (AARG-17-533484).References
1. Fazekas F, Wardlaw JM: The origin of white matter lesions: a further piece to the puzzle. Stroke 2013, 44:951-2.
2. Rosenberg GA: Inflammation and white matter damage in vascular cognitive impairment. Stroke 2009, 40:S20-3.
3. Wardlaw JM, Smith C, Dichgans M: Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. The Lancet Neurology 2013, 12:483-97.
4. Wardlaw JM, Valdes Hernandez MC, Munoz-Maniega S: What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. Journal of the American Heart Association 2015, 4:001140
5. Shi Y, Thrippleton MJ, Makin SD, Marshall I, Geerlings MI, de Craen AJM, van Buchem MA, Wardlaw JM. Cerebral blood flow in small vessel disease: A systematic review and meta-analysis. J Cereb Blood Flow Metab. 2016 Oct;36(10):1653-1667.
6. Cipolla MJ. The cerebral circulation. Integrated systems physiology: From molecule to function. 2009 Jan 1;1(1):1-59.
7. Thomas BP, Liu P, Park DC, van Osch MJ, Lu H: Cerebrovascular reactivity in the brain white matter: magnitude, temporal characteristics, and age effects. Journal of cerebral blood flow and metabolism, 2014, 34:242-7.
8. Rusinek H, Glodzik L, Mikheev A, Zanotti A, Li Y, De Leon MJ: Fully automatic segmentation of white matter lesions: error analysis and validation of a new tool CARS-2013 & Int J Comput Assist Radiol Surg 2013:289-91.
9. Wahlund LO, Barkhof F, Fazekas F, Bronge L, Augustin M, Sjogren M, Wallin A, Ader H, Leys D, Pantoni L, Pasquier F, Erkinjuntti T, Scheltens P, European Task Force on Age-Related White Matter C: A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke 2001, 32:1318-22.
10. Wu D, Ma T, Ceritoglu C, Li Y, Chotiyanonta J, Hou Z, Hsu J, Xu X, Brown T, Miller MI, Mori S. Resource atlases for multi-atlas brain segmentations with multiple ontology levels based on T1-weighted MRI. Neuroimage. 2016 Jan 15;125:120-130.
11. Lu H, Liu P, Yezhuvath U, Cheng Y, Marshall O, Ge Y: MRI mapping of cerebrovascular reactivity via gas inhalation challenges. Journal of visualized experiments : JoVE 2014.
Figures