2363
Long term evaluation of ventricular volume change associated with shunt-responsiveness in idiopathic normal pressure hydrocephalus1Department of Radiology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, 2Department of TELE-Radiology, Bangkok Hospital Headquarters, Bangkok, Thailand, 3Faculty of Physical Therapy, Mahidol University, Bangkok, Thailand, 4Department of Radiological Technology, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand, 5Division of Neurosurgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, 6Department of Preventive and Social Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Synopsis
Shunt surgery is an effective treatment for iNPH, however some patients showed unsustainable response. We investigated how reduction of ventricular size after shunt surgery correlated with clinical outcome, as potential predictor of long-term shunt responsiveness using automated segmentation of ventricular volume from T1W sequence. A reduction of ventricular volume is found to negatively correlate with improved cognition. These findings might be one of helpful imaging predictors for the shunt responders in iNPH.
Introduction
Idiopathic normal pressure hydrocephalus (iNPH) is defined as ventricular dilatation with normal pressure of cerebrospinal fluid (CSF) which is considered as one of treatable cause of dementia effectively treated by shunt surgery. Magnetic resonance imaging (MRI) is one of the tools that implement diagnosis, follow-up and even prediction of clinical outcome in previous research, using various imaging indices. In clinic, a routine visual assessment of ventricular size and Evans’ index, a widely used imaging index to determine ventricular enlargement, shows no significant change after shunt surgery in several studies and not correlated with the actual ventricular volume, which could possibly be the better predictor of the disease according to the pathology1,2. The aim of this study is primarily investigating the long-term ventricular volume changes after shunt surgery and correlation with the long-term clinical outcome as the potential predictor of shunt-responsiveness in iNPH patients.Methods
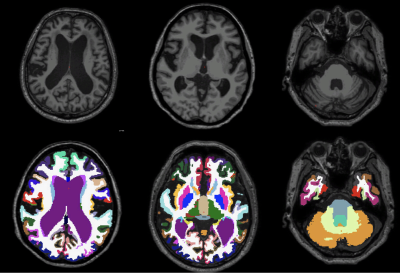
Thirty-one iNPH patients, diagnosed according to revised guideline of iNPH of Japanese Society of NPH, second edition (2012), underwent shunt surgery with available pre- and post-operative MRI. MRI were acquired with a 3T MR scanner with a 32-channel head coil. T1-weighted images were performed using a 3DTurbo Field Echo (TFE) sequence covering the whole brain (field-of-view FOV 230×230×172 mm3, matrix size 352x352, voxel size 0.72×0.72×0.65 mm3, echo time TE /repetition time TR 4.8/9.8 ms; flip angle 8°). Automated whole brain segmentation was performed by using Freesurfer software version 6.0 (http://surfer.nmr.mgh.harvard.edu/). The ventricular volume was segmented into right and left lateral, third and fourth ventricle.Assessment of clinical evaluation before and after shunt surgery, at the available data nearest to MRI, was performed by experienced neurosurgeons using iNPH grading scales (iNPHGS)3, which divided into gait, cognition and urinary disturbance, each domain has 0-4 scales, total of 12 scores for the worst symptoms. The improvement of at least one score in any domain was considered as responsive to shunt surgery. Spearman’s correlation was used to demonstrate association of ventricular volume changes and improvements of iNPHGS.
Results
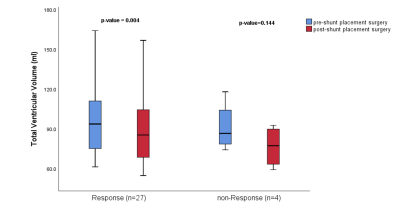
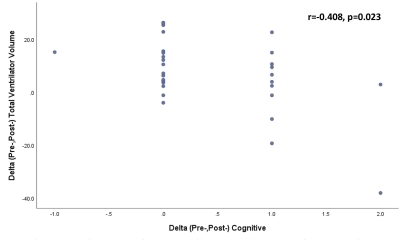
Twenty-seven patients were classified as responders while four patients, having no improvement to post-surgical iNPHGS, were classified as non-responders. Pre-operative MRI with median time of 23 days before surgery (range 6-72 days after excluding outliers) and postoperative MRI with median time of 201 days after surgery (range 97- 811 days) were collected. Pre-operative clinical evaluation was done at median time of 26 days before shunt insertion, range 2-299 days. The clinical evaluation post-operatively was conducted at the nearest time point to post-operative MRI, with the median time of 190 days (6.24 months), range 3-27 months, after shunt insertion.There is a significant decrease of total and lateral ventricular volume after shunt placement surgery in responders' group (p=0.004). There is moderate degree of a significant negative correlation between improved cognition and a reduction in total and lateral ventricular volume. (r=-0.408, p=0.023) While, a weak negative correlation between improved clinical outcome (total iNPHGS scores) and decreased ventricular volume is not statistical significance (r=-0.255, p=0.166).
Furthermore, the symptom duration before shunt surgery is significantly shorter in responders’ group with median time of 12 and 36 months in responders and non-responders, respectively. (p=0.031).
Discussion and conclusion
Long-term ventricular volume decreases significantly among shunt-responders. Also, there is a moderate degree of negative correlation between improved cognition and a reduction in total and lateral ventricular volume. Ventricular volume changes in iNPH may result in alteration of intracranial pressure, brain compliance and cerebral blood flow associated with the cognitive domain. Using ventricular volume as a predictor of treatment response after shunt surgery may be able to reflect a long-term clinical outcome in iNPH patients.Acknowledgements
This research project was supported by Faculty of Medicine, Siriraj Hospital, Mahidol University.References
1. Toma, A. K., Holl, E., Kitchen, N. D., & Watkins, L. D. (2011). Evans' index revisited: the need for an alternative in normal pressure hydrocephalus. Neurosurgery, 68(4), 939–944.
2. Yamada, S., Ishikawa, M., Yamaguchi, M., & Yamamoto, K. (2019). Longitudinal morphological changes during recovery from brain deformation due to idiopathic normal pressure hydrocephalus after ventriculoperitoneal shunt surgery. Scientific Reports, 9.3.
3. Kubo, Y., Kazui, H., Yoshida, T., Kito, Y., Kimura, N., Tokunaga, H. et al. (2007). Validation of Grading Scale for Evaluating Symptoms of Idiopathic Normal-Pressure Hydrocephalus. Dementia and Geriatric Cognitive Disorders, 25(1), 37-45.
Figures
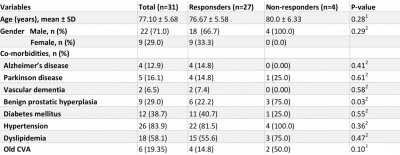
1Independent t-test 2Chi-square test
SD = Standard deviation, CVA = Cerebrovascular accident
Table 1. Demographic data
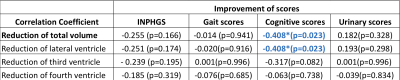
*denotes significant correlation using Spearman’s correlation coefficient
Table 2. Correlation analysis between changes of ventricular volume and clinical scores after shunt placement surgery in iNPH