2353
Clinical value of whole-body diffusion-weighted imaging in evaluation of multiple myeloma1First Hospital of Jilin University, Changchun, China, 2Philips Healthcare, Beijing, China
Synopsis
Whole-body diffusion-weighted imaging (WB-DWI) in the evaluation of bone marrow infiltration in multiple myeloma, and it will be a helpful supplement to the evaluation of multiple myeloma.
Synopsis
This study retrospectively investigated whole-body diffusion-weighted imaging (WB-DWI) in the evaluation of bone marrow infiltration in multiple myeloma.[1, 2] This is a helpful supplement to the evaluation of multiple myeloma.Introduction
Accurate assessment of plasma cell infiltration of the bone marrow supports diagnosis and monitors treatment response in patients with multiple myeloma (MM). This study retrospectively investigated whole-body diffusion-weighted imaging (WB-DWI) in the evaluation of bone marrow infiltration in MM.Materials and Methods
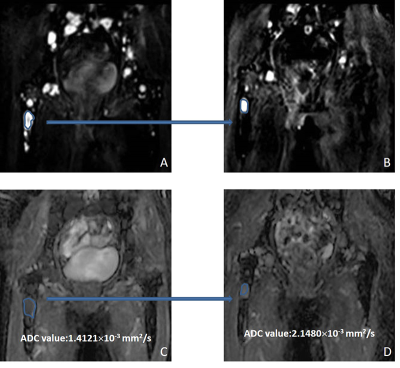
Sixty-eight patients with MM who underwent WB-DWI after treatment were included in the study. Their mean age was 56.91 ±8.57 years and 67.6% were male. Durie-Salmon stage was IIA to IIIB. All Patients with MM were scanned using a 3.0T MR scanner (Ingenia CX, Philips Healthcare, the Netherlands). They underwent WB-DWI between January 2016 and October 2018. Patients received high dose chemotherapy with autologous stem cell transplantation after an induction regimen. Treatment response was assessed by the National Comprehensive Cancer Network guidelines. WB-DWI was performed to measure the apparent diffusion coefficient (ADC) values. The degree of bone marrow infiltration was assessed by bone marrow biopsy within three days of WB-DWI.Result
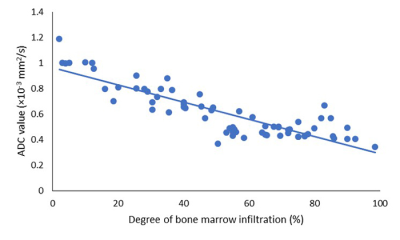
The result was shown in Figure 2. There was a negative correlation between the ADC value and the degree of bone marrow infiltration in the right ilium and this was statistically significant (r=-0.829, P<0.001). Eleven patients also underwent WB-DWI before starting treatment and 10 (91%) had complete response or very good partial response; their ADC values after treatment were significantly higher than those before treatment (P=0.004).Discussion
Related studies have shown that DWI combined with conventional MRI sequences is of great value in the early diagnosis of MM.[3] An important note is that fractures and hemangiomas can also cause high signal intensity on DWI imaging. So, it is important when measuring ADC value, that DWI sequences are considered alongside T2 STIR, mDIXON sequences and medical history. If possible assessment of ADC values in these areas should be avoided, to efficiently reduce design and fabrication errors. Horger et al. suggested that changes in ADC values can be used to detect the initial treatment effect of MM. To a certain extent, the trend of ADC value change can predict the prognosis of the patients. The ADC value of the tumor is in inverse proportion to the density of the cells. Furthermore, the ADC value increases continuously as the tumor burden decreases.[4]In this study, the ADC value of the patients was negatively related to the Infiltration ratio of bone marrow plasmacyte, and the findings was consistent with the principle of WB-DWI imaging. The higher the proportion of immature plasmacyte in the bone marrow, the smaller the intercellular space, the higher degree of water molecules diffusion restriction. In the study by Squillaci et al., DWI showed good agreement with T1 enhancement in ISS staging of MM. Specifically, diffusion-weighted imaging can be used to assess tumor burden relatively accurately.[5] Th is is consistent with the conclusions of Hillengass et al. In another study, Giles et al. found that when the ADC value increased by 3.3% after treatment, the sensitivity of the treatment response assessment to MM was 90% and the specificity was 100%.[6]
Conclusion
The ADC value was negatively correlated with the degree of bone marrow infiltration in the right ilium. In 11 patients also monitored before treatment the ADC values of the largest lesion were shown in Figure 2to increase after treatment.Acknowledgements
None.References
[1] Landgren O, Rajkumar SV. New Developments in Diagnosis, Prognosis, and Assessment of Response in Multiple Myeloma. Clin Cancer Res. 2016. 22(22): 5428-5433.
[2] Rajkumar SV. Multiple myeloma: 2016 update on diagnosis, risk-stratification, and management. Am J Hematol. 2016. 91(7): 719-34.
[3] Puskás T, Henits I. [Use of whole-body diffusion-weighted magnetic resonance imaging for the diagnosis of and therapeutic response in multiple myeloma]. Orv Hetil. 2014. 155(31): 1241-5.
[4] Horger M, Weisel K, Horger W, Mroue A, Fenchel M, Lichy M. Whole-body diffusion-weighted MRI with apparent diffusion coefficient mapping for early response monitoring in multiple myeloma: preliminary results. AJR Am J Roentgenol. 2011. 196(6): W790-5.
[5] Squillaci E, Bolacchi F, Altobelli S, et al. Pre-treatment staging of multiple myeloma patients: comparison of whole-body diffusion weighted imaging with whole-body T1-weighted contrast-enhanced imaging. Acta Radiol. 2015. 56(6): 733-8.
[6] Giles SL, Messiou C, Collins DJ, et al. Whole-body diffusion-weighted MR imaging for assessment of treatment response in myeloma. Radiology. 2014. 271(3): 785-94.
Figures