2337
Multiparametric MRI of rectal cancer patients for early detection of therapeutic efficacy of neoadjuvant radio-chemotherapy1Medizinische Fakultät, Universität Freiburg, Freiburg, Deutschland, Radiologische Klinik, Medizinphysik, Universitätsklinikum Freiburg, Freiburg, Germany, 2Klinik für Radiologie, Klinikum St. Georg Leipzig, Leipzig, Germany
Synopsis
Significant changes of tumor properties during and after neoadjuvant radiochemo therapy are observed in DCE- as well as in DWI-MRI. However heterogneiity of the patient cohort impede more clear results. To overcome this an increase in patient numbers may allow to gain significant results for sharper definied sub groups. This will include combining single results of DCE- and DWI.MRI data in a more integral approach to increase the predictive value.
Introduction
For patients with advanced rectum carcinoma neoadjuvant radiochemo therapy is integral part of a standard therapy plan. A quarter of the patients show complete response. However a significant share of patients, up to 50%, shows no response at all. Patient selection for suitable treatment paths is challenging1. This raises the need of an early indicator to identify potential non responder to allow an early therapy change, which is in the interest of the patient as well as the health care system. Imaging plays a vital role informing this decision-making process, both by providing prognostic details about the cancer before the start of treatment and by updating this picture as the cancer responds or fails to respond to treatment2. MRI became the gold standard in rectal cancer imaging3. Its extension with functional MRI like diffusion weighted MRI (DWI-MRI) and dynamic contrast enhanced MRI (DCE-MRI) may help to gain information for patient selection. It was shown that diffusion weighted MRI may detect treatment-induced changes in tumor cell membrane integrity well before any volumetric decrease4. A general multiparametric MRI biomarker approach for early cancer therapeutic response assessment was presented by Galbán et al5 which was then applied to different types of cancer.Methods
In this study 55 patients with locally advanced rectal cancer were enrolled. They all underwent neoadjuvant radiochemo therapy. MRI scans were applied before, 48hours, 2, 4 and 12 weeks after treatment start. Additional to standard morphological MRI scans the protocol included diffusion weighted MRI and dynamic contrast enhanced MRI scans. All MRI scans were acquired on a 3-T Siemens Trio MRI system (Erlangen, Germany) using body and spine array coils. Contours were manually drawn over tumors as delineated on T2-weighted, T1-weighted or contrast enhanced images. For each measurement a single slice were analyzed in maximal tumor extent. For the resultant images DCE-parameter ( semi-quantitatively w. Brix compartment model) and ADC values were calculated. Histopathologic data were additionally collected. Patients were divided in groups according to their regression grade after therapy (class 1 Rg 0-49%, class 2 Rg 50≥75%, class 3 RG 75>90% , class 4 Rg >90%).Results
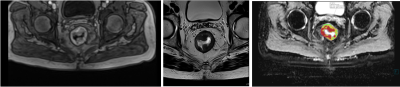
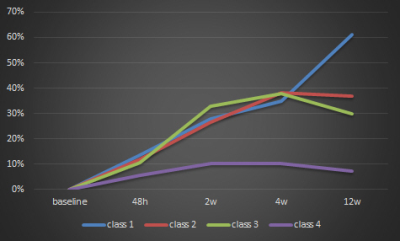
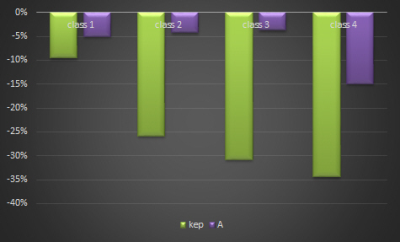
Figure 1 exemplary shows a T1 weighted image out of the DCE-MRI time series, a T2 weighted image as well as a ADC-map of a patient with advanced rectum carcinoma. Absolute ADC values only showed difference at baseline for patients with strong regression, but were indifferent at other time points. However %-difference of ADC values at follow up examinations versus baseline differed. This is shown in Figure 2. Patients with no or minimal regression (class 1-3) show an strong increase in ADC over the time, while patients with strong regression (class4) only showed a minimal increase followed by a slight decrease of ADC over time. Derived from DCE-MRI data, kep (transfer rate) and A (amplitude) both displayed an increasing decrease with increasing regression grade which is plotted in Figure 3.Discussion and Conclusion
Significant changes of tumor properties during and after neoadjuvant radiochemo therapy are observed in DCE- as well as in DWI-MRI. However heterogneiity of the patient cohort impede more clear results. To overcome this an increase in patient numbers may allow to gain significant results for sharper definied sub groups. The next step will include combining single results of DCE- and DWI.MRI data in a more integral approach to increase the predictive value.Acknowledgements
This study was supported by the ‘Deutsche Krebshilfe’; Funding code 110724.References
1. Allalx ME et al., Ann Surg On col 2013;20:2921-2928.
2. Hunter, C. Expert Review of Gastroenterology & Hepatology 2016, 10, 1011–1025
3. Brown G, Proc. Intl. Soc. Mag. Reson. Med. 22 (2014) 0004.
4 Schepkin VD et al. Magn Reson Imaging. 2006 April ; 24(3): 273–278.
5. Galbán C, Tomography. 2015 September ; 1(1): 44–52.
Figures