2326
MRI Role in Evaluation of T staging and Lymphatic metastases for Esophageal Cancer1The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China, 2MR Scientific Marketing, Siemens Healthcare, Guangzhou, China
Synopsis
Esophageal cancer ranks seventh in terms of incidence and sixth in mortality among all cancers. Accurate staging of esophageal cancer helps to choose appropriate therapeutic strategy. Current imaging modalities used for evaluating esophageal cancer have their own disadvantages. Therefore, we compared MRI, which is non-invasive, non-radiating and of high soft-tissue resolution, with EUS in preoperative T staging and with PET/CT in preoperative lymphatic metastases of esophageal cancer. In this study, MRI showed higher sensitivity, specificity and accuracy in T staging, while MRI and PET/CT showed similar performance in lymph nodes evaluation.
Introduction
Esophageal cancer (EC) is the seventh most common cancer worldwide with poor prognosis. Different therapeutic strategies are used according to different tumor stages, so accurate evaluation of EC has a great importance [1-3]. Endoscopic ultrasonography (EUS) has been widely used to evaluate T staging of EC, which is considered as the most credible tool [4]. Positron emission tomography/ computed tomography (PET/CT) is usually used for detecting lymph node metastases of EC [5]. But EUS is invasive and PET/CT is radiating. Compared with these two modalities, magnetic resonance imaging (MRI) is non-radiating and non-invasive, which can potentially be useful in T staging and the diagnosis of lymph node metastases due to the high-resolution soft tissue images on BLADE T2-weighted imaging and radial VIBE imaging. However, there is no report on the accuracy of MRI in evaluation of lymph node metastasis of EC compared with PET/CT. Therefore, this study aimed to evaluate the performance of MRI in preoperative T staging and preoperative diagnosis of lymphatic metastases in EC using a combined method of BLADE T2-weighted and radial VIBE images, compared with EUS and PET/CT, respectively.Methods
This study enrolled 21 EC patients (19 males and 2 females; mean age, 63.9 years; range, 42-77 years) who underwent MRI and EUS examinations within 14 days before surgery. Among them, 13 patients (13 males; mean age, 62.6 years; range, 43-77 years) underwent PET/CT at the same time. All patients underwent MR scans on a 3-T scanner (MAGNETOM Vida, Siemens Healthcare, Erlangen, Germany) with an anterior 18-element body coil and in-built posterior 32-element spine coil array. The patients were positioned head-first supine. Gadobutrol (0.1 mmol/kg; Bayer AG, Berlin, Germany) was injected at a rate of 1.5 mL/s by an MR high pressure injector (Medtron AG, Saarbrücken, Germany). A T2-weighted TSE-BLADE sequence and a post-contrast free-breathing 3D T1-Weighted radial VIBE sequence were used for evaluation of EC. The T2-BLADE images were acquired with the following parameters: TR/TE = 3000/97 ms, FOV = 220 × 220 mm2, slice thickness = 3 mm, voxel size = 0.7 × 0.7 × 3.0 mm3, 36 slices. The radial VIBE images were obtained after the contrast injection using the following parameters: TR/TE = 2.90/1.38 ms, FOV = 300 × 300 mm2, slice thickness = 1 mm, voxel size = 1.0 × 1.0 × 1.0 mm3, 128 slices.Two experienced radiologists randomly evaluated all the patients’ images by consensus and they were blinded to clinical and other imaging information about patients. All MR images were evaluated according to the 8th edition American Joint Committee on Cancer (AJCC) TNM Classification for EC: T0-T1, no lesions or tumor is confined in mucosa and submucosa; T2, tumor invades muscularis propria but without breaking through it; T3, tumor invades adventitia; T4a, tumor invades pleura, pericardium or diaphragm [6]. Pathology was considered the gold standard. The accuracy, sensitivity and specificity were calculated to evaluate the performance of the T staging of MRI and EUS, and preoperative lymphatic metastases of MRI and PET/CT in EC.
Results
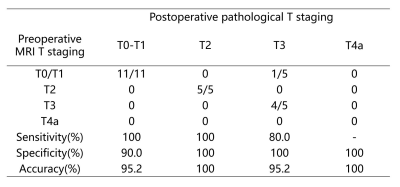
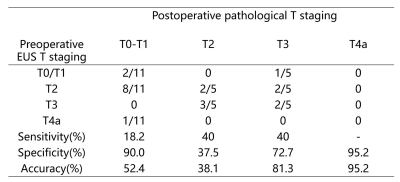
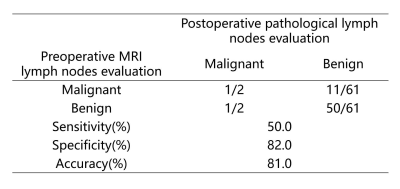
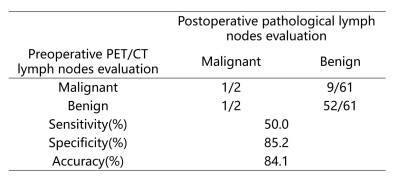
Images of T1, T2 and T3 stage cases were shown in the Figure 1. The statistics of pathological T staging, MRI and EUS in T staging of EC was shown in Table 1-2. Comparison between MRI and pathological lymph nodes evaluation, as well as PET/CT and pathological lymph nodes evaluation was shown in Table 3-4.Discussion and conclusion
MRI showed higher sensitivity (range, 80%-100%), specificity (range, 90%-100%) and accuracy (range, 95.2%-100%) than those of EUS (sensitivity ranged from 18.2%-40%, specificity 37.5%-95.2% and accuracy 38.1%-95.2%) in T staging of EC. As for lymph nodes evaluation, sensitivity (50%, 50%), specificity (82%, 85.2%) and accuracy (81%, 84.1%) of MRI are comparable to those of PET/CT. Therefore, MRI as a non-invasive, non-radiating tool, may be a better choice for the T staging and preoperative diagnosis of lymphatic metastases in EC using a combined method of T2-BLADE and radial VIBE. However, the sample size of this study was small. And a larger sample size may be needed for further research.Acknowledgements
No acknowledgement found.References
1. Rice TW, Gress DM, Patil DT, et al. Cancer of the esophagus and esophagogastric junction-Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017; 67(4):304-317.
2. Kato H, Nakajima M. Treatments for esophageal cancer: a review. Gen Thorac Cardiovasc Surg. 2013; 61(6):330-335.
3. Shapiro J, van Lanschot JJB, Hulshof MCCM, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015; 16(9):1090-1098.
4. Luo LN, He LJ, Gao XY, et al. Endoscopic ultrasound for preoperative esophageal squamous cell carcinoma: a meta-analysis. PLoS One. 2016; 11(7): e0158373.
5. Hu J, Zhu D, Yang Y. Diagnostic value of 18F-fluorodeoxyglucose positron-emission tomography/computed tomography for preoperative lymph node metastasis of esophageal cancer: A meta-analysis. Medicine (Baltimore). 2018; 97(50): e13722.
6. Amin MB, Edge SB, Greene FL, et al. The AJCC Cancer Staging Manual, 8th Edition.
Figures
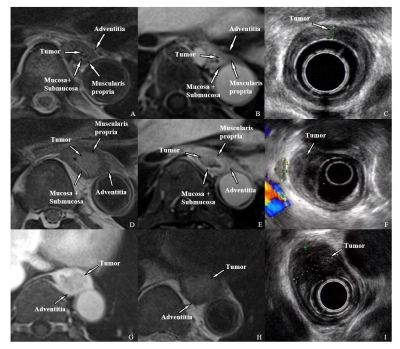
Figure1. MRI and EUS images of T1-T3 esophageal cancer. T1: A-C, T2WI BLADE(A), Enhanced T1WI radial VIBE(B), and EUS(C). The tumor located in the mucosa and submucosa and protrudes into the lumen without muscularis propria invasion. T2: D-F, T2WI BLADE(D), Enhanced T1WI radial VIBE(E), and EUS(F). The tumor breaks through the submucosa and is limited to the muscularis propria. T3:G-I, T2WI BLADE(G), Enhanced T1WI radial VIBE(H), and EUS(I). The tumor is confined to the adventitia.