Gang FENG1, Mingxiang Sun1, Liling Peng1, Zhaoting Meng1, and Xin Gao1
1Shanghai Universal Medical Imaging Diagnostic Center, Shanghai, China
Synopsis
To explore the value of assessing pancreatic
cancers with integrated positron emission tomography (PET)/magnetic resonance
imaging (MRI), fluorine-18 fluorodeoxyglucose (FDG) PET and diffusion weighted
imaging (DWI) were applied. Integrated PET/MR is a promising and powerful tool
for pancreatic tumor detection and assessment. It is relatively advantageous to
combine PET and DWI together to discriminate malignant tumors from benign
lesions.
INTRODUCTION
To explore the value of assessing pancreatic
cancers with integrated positron emission tomography (PET)/magnetic resonance
imaging (MRI), fluorine-18 fluorodeoxyglucose (FDG) PET and diffusion weighted
imaging (DWI) were applied to discriminate malignant pancreatic tumors from
benign lesions.METHODS
The local ethics committee has approved this study.
Written, informed consent was obtained. A cohort of 56 subjects suspected with pancreatic
lesions who accepted PET/MR scans in our center from Jan. 2016 to Dec. 2019
were retrospectively collected in this study. Several subjects were excluded
based on some reasons, four subjects for being little FDG uptake shown, three with
accessory spleen for ADC being merely measureable, six with little metabolic
tumor volume (MTV) (<10 cm3) or total lesion glycolysis (TLG<10). Among the 45
valid subjects (age 60.55±2.05, 30 males and 15 females), 37 (age 50.00±2.82) were
finally diagnosed with malignant tumors, eight (age 60.55±2.06) were with
benign lesions. All diagnosis were confirmed later by biopsy/surgery. The interval between
PET/MRI scans and biopsy/surgery of each subject was shorter than one month.
Both PET and MRI measurements were performed
simultaneously on an integrated whole-body PET/MRI scanner (Biograph mMR,
Siemens Healthcare, Erlangen, Germany). PET data acquisition started 60 min
after the injection of 18F-FDG (3.7 MBq/Kg). Each subject had a fasting of six
hours before FDG injection. MRI data acquisition was simultaneously on during
PET measurement. Delineation of ROIs was manually done along the edge of the
lesions slice by slice by three experienced experts with both radiology and nuclear
medicine background on Syngo Via platform (Siemens Healthcare, Erlangen,
Germany). The minimum apparent diffusion coefficient (ADCmin) and maximum standardized
uptake value (SUVmax) values were measured subsequently. Statistical Package
for the Social Sciences (version 20; SPSS, Chicago, IL) and Matlab 2014b (MathWorks,
Natick, MA) were used for statistical calculations.
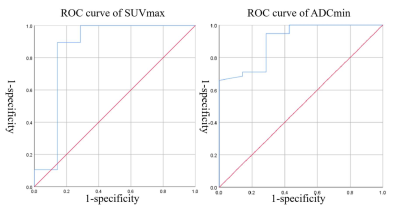
Receiver operating characteristic (ROC) curve was
applied to speculate the sensitivity, specificity, positive predictive value (PPV),
negative predictive value (NPV) and accuracy of diagnosis. Spearman's rank
correlation coefficient between SUVmax and ADCmin was calculated. To combine
PET and DWI parameters together in diagnosis to yield a systematic result, it
is supposed that subject with negative results both from PET and DWI will be asserted
as with benign lesion, otherwise it is suspected with malignant tumors.RESULTS
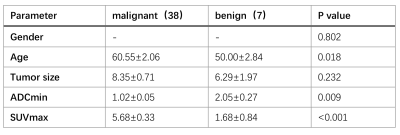
No significant difference was found between malignant
and benign tumors of gender (p = 0.802) or tumor size (p = 0.232) while a significant
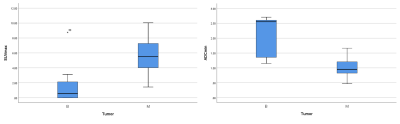
difference of age (p = 0.018) was found (table 1). The values of ADCmin and SUVmax
are 1.02±0.05, 5.68±0.33 of malignant tumors and 2.05±0.27, 1.68±0.84 of benign
lesions (figure 1). The difference of ADCmin and SUVmax are both significant (the
p values are 0.009 and <0.001 respectively).
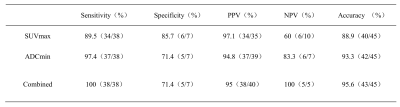
The results of ROC analysis are mentioned in table 2.
Thresholds of SUVmax and ADCmin are 3.2 (Youden Index = 0.752) and 1.145 (Youden
Index = 0.658). Compared with SUVmax, ADCmin has a higher Sensitivity (97.4% VS.
89.5%) but a lower Specificity (71.4% VS. 85.7%). SUVmax has a slightly higher
potential to predict positive results (PPV = 97.1%) than ADCmin (PPV = 94.8%)
while its negative predictive value (NPV = 60%) is lower than that of ADCmin (NPV
= 83.3%). And as a summary of diagnosis accuracy, ADCmin is slightly better
than SUVmax (93.3% VS. 88.9%).
Table 2 shows that the result of combining SUVmax
and ADCmin for diagnosis is more promising than each standalone. The accuracy
was raised to 95.6% and NPV to 100%. PPV is 95%. The sensitivity is now 100%
while the specificity has a drop off (specificity = 71.4%) from applying SUVmax
individually.
A significant negative relationship was found
between ADCmin and SUVmax via Spearman's rank correlation coefficient (R =
-0.525, p < 0.001).DISCUSSION
Previous studies of pancreatic cancers based on PET
or PET/CT gave a series of diagnostic performance. M T Keogan et al. got sensitivity
of FDG PET for revealing malignant disease in the pancreas 88% and specificity 83%
in their study1. The study of S.P. Kauhanen et al. in FDG-PET/CT
gave a diagnostic accuracy is 79%2. J. M. Farma et al. got sensitivity and specificity
of diagnosis with PET/CT 89% and 88% while sensitivity of detecting metastatic
disease 61%3. The result of this study shows it is relatively advantageous
to combine FDG-uptake and diffusion parameters together for
pancreatic tumor assessment.
Fifteen subjects out of 38 found no hepatic, pulmonary, lymphatic or osseous
metastasis before PET/MR scans. The PET/MR scans helped to find two with peritoneal
metastasis, one with multiple pulmonary metastasis, one with multiple osseous metastasis
and 11 with retroperitoneal lymph node metastases with a simultaneous hepatic metastases
and/or metastases to the rest of the body. The results based on PET/MR lead to amendments
of treatment protocols of 12 patients, who avoided unnecessary surgeries.
The integrated 18F-FDG PET/MRI has advantages of non-ionizing radiation,
multi-modality and multi-parameter imaging. It is a better method to identify benign and malignant pancreatic lesions.
For lesions without uptake FDG, contrast-enhanced scans are required to assist
histological diagnosis.CONCLUSION
Integrated PET/MR is a promising and powerful tool
for pancreatic tumor detection and assessment. It is relatively advantageous to
combine PET and DWI together to discriminate malignant tumors from benign
lesions.Acknowledgements
This study was supported by the Special Fund for artificial Intelligence Innovation and Development of Shanghai Economic and Information Technology Commission 2019-RGZN-01079 and UV Clinic Research Fund UV2020Z02References
[1] Keogan MT, Tyler D, Clark L, Branch MS,
McDermott VG, DeLong DM, Coleman RE. Diagnosis of pancreatic carcinoma: role of
FDG PET. AJR Am J Roentgenol. 1998 Dec;171(6):1565-70. doi:
10.2214/ajr.171.6.9843289. PMID: 9843289.
[2] Kauhanen SP, Komar G, Seppänen MP, Dean KI,
Minn HR, Kajander SA, Rinta-Kiikka I, Alanen K, Borra RJ, Puolakkainen PA,
Nuutila P, Ovaska JT. A prospective diagnostic accuracy study of
18F-fluorodeoxyglucose positron emission tomography/computed tomography,
multidetector row computed tomography, and magnetic resonance imaging in
primary diagnosis and staging of pancreatic cancer. Ann Surg. 2009
Dec;250(6):957-63. doi: 10.1097/SLA.0b013e3181b2fafa. PMID: 19687736.
[3] Farma JM, Santillan AA, Melis M, Walters J,
Belinc D, Chen DT, Eikman EA, Malafa M. PET/CT fusion scan enhances CT staging
in patients with pancreatic neoplasms. Ann Surg Oncol. 2008 Sep;15(9):2465-71.
doi: 10.1245/s10434-008-9992-0. Epub 2008 Jun 13. PMID: 18551347.