2273
Comparison of Respiratory-Gating Weighting Algorithms in Neonatal Pulmonary UTE-MRI1Department of Radiology, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States, 2Pulmonary Medicine, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States, 3Department of Medical Physics, University of Wisconsin, Madison, WI, United States
Synopsis
Pulmonary 1H ultrashort echo-time (UTE)-MRI provides clinically relevant structural information in neonates with lung disease of prematurity (bronchopulmonary dysplasia, BPD) and has strong, unexplored potential to evaluate regional pulmonary function. Retrospective respiratory-gated UTE-MRI allows reconstructed images from different phases of the breathing cycle. Here, we compared four retrospective gating approaches in 3 BPD subjects with different weighted time intervals: 1 hard-gating and 3 soft-gating (exponential, inverse and linear weighting functions). Overall, linearly weighted soft-gating provided better compromise between apparent SNR (aSNR) and motion-blurring. This optimized respiratory-gating approach opens the door for improved understanding of regional pulmonary function deficits in neonates.
Introduction
Neonates born prematurely often suffer from severe and chronic lung disease (bronchopulmonary dysplasia, BPD). Pulmonary 1H ultrashort echo-time (UTE)-MRI can provide 3D proton-density-weighted images of structural lung pathologies and predict clinical outcomes in neonatal BPD1,2; these MR images have spatial resolution comparable to CT but avoid radiation exposure3, do not require sedation/anesthesia for breathing maneuvers – all important considerations for procedures in neonates with delicate respiratory status. While free-breathing UTE-MRI of lung structures in BPD have clinical relevance, the pulmonary functional information available from 1H UTE-MRI in infants remains largely unexplored.Retrospective respiratory-gating of tidal-breathing UTE-MRI, via the motion-modulated k0 time-course, allows images to be reconstructed during different phases of the respiratory cycle, creating cine-like images from a single acquisition4. A variety of respiratory gating approaches that make use of different weighted time-intervals have been suggested, including hard-gating (reconstructing images using only data acquired during the period of interest) and soft-gating (reconstructing images using all data, with weight based on proximity to the period of interest). Each approach has trade-offs between various image quality metrics, including signal-to-noise ratio (SNR) and reduction of motion blur; hard-gating yields lower scan-efficiency/SNR since large intervals of data are discarded, whereas soft-gating yields improved scan-efficiency/SNR due to non-zero weighting of data outside the bin of interest. Various weighting algorithms for soft-gating have been published in the literature, such as improved least squares-based5 and L1-ESPIRiT6. However, these algorithms have not been compared to evaluate the trade-off between SNR and temporal accuracy of reconstruction. Here, we assess three weighting algorithms in soft-gated reconstructions of 1H lung MRI in 3 preterm neonates with BPD lung disease, compared with a hard-gated approach.
Methods
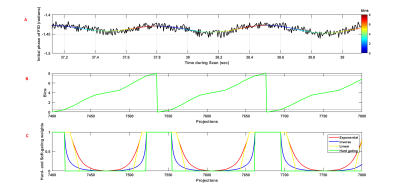
3D radial UTE spoiled gradient echo (SPGR) was acquired on a neonatal-sized 1.5T MRI scanner (hardware: ONI Medical Systems, Wilmington, MA; software: GE Healthcare, Waukesha, WI)7 with pseudo-randomized sampling and variable density readout trajectories8. UTE parameters were: TE=~200μs; TR=~5.2ms; FA=5°; FOV=18cm; number of radial projections=~200,000; 3D isotropic resolution 0.7mm; and duration =~16min.As previously published, the motion-modulated k0 time-course was used to retrospectively generate a respiratory-tracking waveform4. A smoothed waveform was obtained after applying a low-pass filter and waveform data that did not represent respiratory motion due to bulk motion was discarded. All remaining data points were assigned to one of 8 bins (0-7), representing a specific phase of the respiratory cycle (e.g., end-expiration, peak inhalation). (Figure 1A).
Gated images were reconstructed using a hard-gating algorithm where each bin was assigned data based on the amplitude of each breathing cycle. Three soft-gating weighting algorithms: least-squares, an inverse function for weighting values with data points on the respiratory cycle (modified from Samsonov et al.5); L1-ESPIRiT, an exponential function (modified from Larson et al.6); and linear weighting. Two parameters controlled the weighting functions: threshold (the width of the region given maximum weighting) and slope (the rate at which the weighting decreased outside the region of interest).
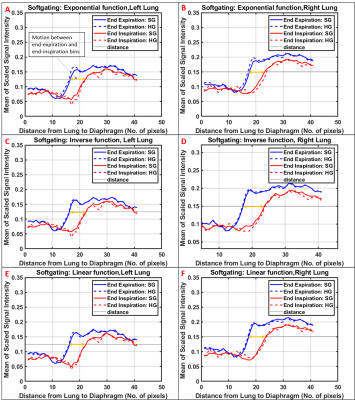
To compare image quality between hard-gating and the three soft-gating weighting algorithms, the following three metrics were chosen: aSNR (apparent SNR, defined as the mean signal of the region of interest, divided by the standard deviation of signal outside the region of interest); gradient of the signal intensity superior-inferior line profile across the lung-diaphragm barrier (mean of ≥10 pixels in the left-right direction); and distance (voxels) between end-expiration and end-inspiration line intensity profiles for motion estimation.
Results
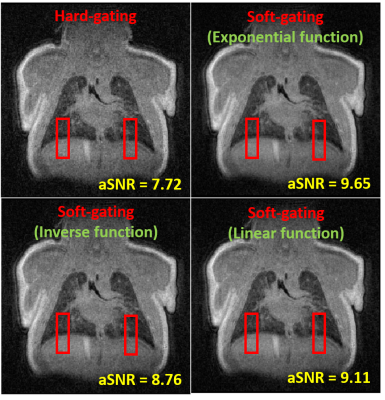
Representative coronal slices from each of the weighting algorithms are shown in Figure 3. The optimal parameters for the three soft-gating weighting functions were: (1) Exponential function: threshold=1, slope=1; (2) Inverse function: threshold=1, slope=0.2; and (3) Linear function: threshold=1, slope=2.Figure 4 summarizes the three image quality evaluation metrics produced using the optimal reconstruction parameters. All soft-gating reconstructions yielded higher aSNR than hard gating. The exponential function produced the highest aSNR. The inverse and linear functions produced sharper images with reduced diaphragmatic motion blurring compared to the exponential function.
The exponential and linear soft gating reconstructions produced the highest average gradient of the signal intensity through the lung-diaphragm boundary across both lungs.
Discussion
The optimal soft-gating weighting algorithm maximizes aSNR, while minimizing motion blur caused by including data from outside the period of interest. The limits for these measures are the aSNR of the ungated image, which includes all data, and the sharpness of the hard-gated image, which has minimal motion blurring.Our results demonstrate that exponential weighting provides the highest aSNR (25% higher than hard gated); however, it suffers from motion blur at the diaphragm over 1-2 voxels more than hard gating. Similar tradeoffs are shown for the inverse function, which reduced motion blurring but resulted in a lower aSNR; the linear weighting function, which provided an aSNR 18% higher than hard gating, with reduced motion blurring. These results demonstrate that optimized linearly- and exponentially weighted soft-gating functions provide the best compromise between aSNR and motion blur at the lung-diaphragm boundary, as compared with hard-gating and inversely weighted soft-gating.
Conclusion
Optimized soft-gating weighting allows reconstruction of respiratory cine-images from neonatal chest UTE MRI at higher aSNR (13.5-25%) with minimal motion blurring sacrifice. This offers promising potential for evaluating abnormal pulmonary function in neonates with lung disease.Acknowledgements
No acknowledgement found.References
1. Higano NS, Fleck RJ, Spielberg DR, et al. Quantification of neonatal lung parenchymal density via ultrashort echo time MRI with comparison to CT. J Magn Reson Imaging. 2017. doi:10.1002/jmri.25643
2. Higano NS, Spielberg DR, Fleck RJ, et al. Neonatal pulmonary magnetic resonance imaging of bronchopulmonary dysplasia predicts short-term clinical outcomes. Am J Respir Crit Care Med. 2018. doi:10.1164/rccm.201711-2287OC
3. Miglioretti DL, Johnson E, Williams A, et al. Pediatric Computed Tomography and Associated Radiation Exposure and Estimated Cancer Risk. 2017;167(8):6-14. doi:10.1001/jamapediatrics.2013.311.Pediatric
4. Higano NS, Hahn AD, Tkach JA, et al. Retrospective respiratory self-gating and removal of bulk motion in pulmonary UTE MRI of neonates and adults. Magn Reson Med. 2017. doi:10.1002/mrm.26212 5. Johnson KM, Block WF, Reeder SB, Samsonov A. Improved least squares MR image reconstruction using estimates of k-Space data consistency. Magn Reson Med. 2012;67(6):1600-1608. doi:10.1002/mrm.23144
6. Jiang W, Ong F, Johnson KM, et al. Motion robust high resolution 3D free-breathing pulmonary MRI using dynamic 3D image self-navigator. Magn Reson Med. 2018;79(6):2954-2967. doi:10.1002/mrm.26958
7. Tkach JA, Hillman NH, Jobe AH, et al. An MRI system for imaging neonates in the NICU: Initial feasibility study. Pediatr Radiol. 2012. doi:10.1007/s00247-012-2444-9
8. Hahn AD, Higano NS, Walkup LL, et al. Pulmonary MRI of neonates in the intensive care unit using 3D ultrashort echo time and a small footprint MRI system. J Magn Reson Imaging. 2017. doi:10.1002/jmri.25394
Figures