2247
Grading of pediatric intracranial tumors: are intravoxel incoherent motion and diffusion kurtosis imaging superior to conventional DWI?1The First Affiliated Hospital of Fujian Medical University, Fujian Fuzhou, China, 2SIEMENS healthcare diagnostic imaging, Shanghai, Pudong, Zhouzhu Highway 278, China, 3SIEMENS Healcare, Erlangen, Germany
Synopsis
To explore the correlations between parameters derived from conventional diffusion-weighted imaging (DWI), intravoxel incoherent motion (IVIM), and diffusion kurtosis imaging (DKI) with histopathologic features of pediatric intracranial tumors.
Introduction
Pediatric intracranial tumors (PIT) are the second most common cancers with the highest mortality among children1. Conventional diffusion-weighted imaging (DWI), which assumes that water molecular diffusion follows a Gaussian distribution, could noninvasively provide additional functional information within tumor2. However, the ADC value calculated using the monoexponential model may not accurately reflect the water molecular diffusion behaviour due to the influence of capillary microcirculation and complex cellular microstructural barriers within tumor. Previous researchers have suggested that intravoxel incoherent motion (IVIM) and diffusion kurtosis imaging (DKI) might provide a more accurate illumination of water molecular diffusion behaviour3-5. Therefore, the aim of this study is to explore the correlations between parameters derived from conventional DWI, IVIM, and DKI with histopathologic features of pediatric intracranial tumors.Methods
Fifty-seven pediatric patients with histologically proved intracranial tumors underwent conventional DWI, IVIM and DKI were recruited in this study. All patients underwent MR examinations with a 3T MR scanner (Magnetom Skyra, Siemens Healthcare, Erlangen, Germany) using a 20-channel head/neck coil. Routine MR sequence were conducted, including axial T2-weighted imaging, axial susceptibility weighted imaging, and pre- and post-contrast axial T1-weighted imaging. Multiple b-values DWI was performed using a single-shot echo planar imaging sequence in the axial plane. The detailed imaging parameters were as follow: repetition time/echo time=5000 ms/78 ms, field of view = 220 mm×220 mm, acquisition matrix = 150 × 135, parallel acceleration factor = 2, slice thickness = 5 mm, gap = 1 mm and acquisition time=8 min 25 s. 13 different b values (b = 0, 50, 100, 150, 200, 300, 400, 600, 800, 1000, 1400 and 2000 s/mm2 with number of signal averages of 2, 2, 2, 2, 2, 2, 2, 2, 2, 3, 3, 4, 4, respectively) were applied.For post-processing, the conventional DWI [apparent diffusion coefficient (ADC)], IVIM [pure diffusion coefficient (D), pseudo-diffusion coefficient (D*) and perfusion fraction (f)] and DKI [diffusion kurtosis (K) and diffusion coefficient (Dk)] parameters were calculated using a prototype software (Body diffusion toolbox, Siemens Healcare, Erlangen, Germany), and the quantitative diffusion values in the solid component of tumors were measured. Histopathologic features, including cellularity, Ki-67, and microvessel density were measured. These parameters were compared between the low-and high-grade pediatric intracranial tumors by using the Mann-Whitney U test. Spearman correlations, receiver-operating characteristic analysis, and multiple logistic regression were performed.
Results
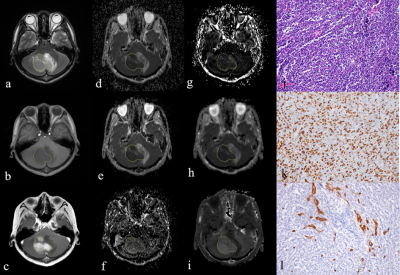
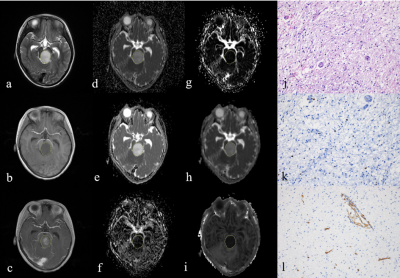
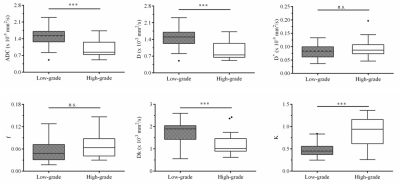
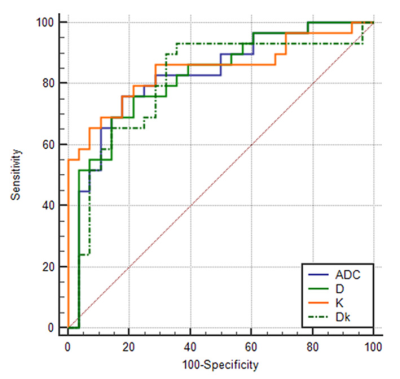
The the calculated diffusion parameters of two representative patients were also shown (Figure 1 and 2). The ADC, D and Dk values were lower, whereas K value was higher in high-grade pediatric brain tumors than those in low-grade pediatric brain tumors (all p <0.05). The K value was positively correlated with the cellularity and Ki-67 (rho = 0.656~0.752), while the ADC, D and Dk values were negatively correlated with the cellularity and Ki-67 (rho = -0.514~-0.698). The AUC values of ADC, D, Dk and K values were 0.825, 0.821, 0.804, and 0.846 for differentiating high-grade from low-grade pediatric brain tumors, respectively. A higher K value (K > 0.745) independently predicted a high-grade pediatric intracranial tumors [odds ratio (OR) = 40.29, p <.001].Discussion & Conclusions
Compared with other diffusion metrics, K value may serve as the strongest independent factor for predicting pediatric intracranial tumors grade. Moreover, the diffusion metrics may potentially reflect tumor cellularity and Ki-67.Acknowledgements
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subjectmatter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary forthis paper. Institutional Review Board approval was not required because this was a retrospective study. No study subjects or cohortshave been previously reported.References
1.Ward E, DeSantis C, Robbins A, Kohler B, Jemal A (2014) Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin 64:83-103
2. Koral K, Mathis D, Gimi B et al (2013) Common pediatric cerebellar tumors: correlation between cell densities and apparent diffusion coefficient metrics. Radiology 268:532-537
3.Le Bihan D (1988) Intravoxel incoherent motion imaging using steady-state free precession. Magn Reson Med 7:346-351
4.Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161:401-407
5.Jensen JH, Helpern JA, Ramani A, Lu H, Kaczynski K (2005) Diffusional kurtosis imaging: the quantification of non-gaussian water diffusion by means of magnetic resonance imaging. Magn Reson Med 53:1432-1440
Figures