2159
The value of contrast enhanced T2 FLAIR in the differential diagnosis of intracranial ring-enhanced lesions1Affiliated Hospital of Guilin Medical University, Guilin, China, 2MR Research, GE Healthcar, Beijing, China
Synopsis
The goal of current study is to validate whether the contrast enhanced T2 FLAIR (CE-T2-FLAIR) could provide additional value for clinical diagnosis beyond the regular sequence. A retrospective analysis of 52 cases of intracranial ring-enhanced lesions validated by menstrual surgery, pathology or clinical follow-up observation from January 2019 to June 2020 was performed in current study. Our results demonstrated that the CE-T2-FLAIR "edge enhancement sign" was more closely related to inflammatory lesions, and indicated a high possibility of that disease.
Introduction
Intracranial ring-enhancing lesions are relatively common clinical imaging manifestations, but its differential diagnosis is often challenging [1]. There are various causes for intracranial ring-enhancing lesions. As for patients with normal immune function, the common causes include glioma, intracranial metastases, infectious diseases, demyelinating diseases, and brain contusions. With regard to immunosuppressed patients, toxoplasmosis, primary central nervous system lymphoma, fungal infectious diseases may cause intracranial ring-enhancing lesions [2]. In addition, T2-FLAIR is a special reversal recovery pulse sequence with longer TR, TE, IR, and contrast-enhanced T2-FLAIR (CE-T2-FLAIR) has demonstrated its capacity for differentiating Meningitis and multiple brain metastases [3-6]. Hence, we hypothesized that the CE-T2-FLAIR may provide more information for differential diagnosis of primary central nervous system lesions than conventional contrast-enhanced T1WI (CE- T1WI).Methods
52 patients (49.5±19.0 years old, 31 males) with an intracranial ring-enhanced lesion were scanned on a 3T MRI scanner using a 32-channel sensor head coil. The MRI scan protocol included T1WI, T2WI and T2-FLAIR, and sagittal T2WI. The enhanced MRI scan used rapid injection of gadolinium meglumine (Gd-DOTA) through the elbow vein. Thereafter, the CE- T1WI and CE-T2-FLAIR were performed. Two radiologists independently assessed and recorded the occurrence rate of the CE-T2-FLAIR “marginal enhancement sign” without knowing the pathological results. The final pathological or follow-up results were used as the standard to estimate the consistency of the diagnosis of the two diagnosing doctors. Last, the chi-square test was applied to analyze whether it is statistically significant.Results
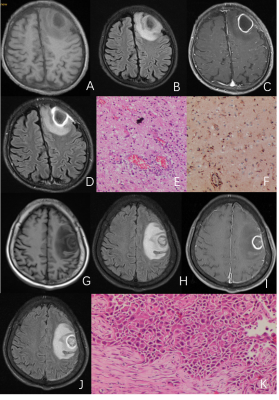
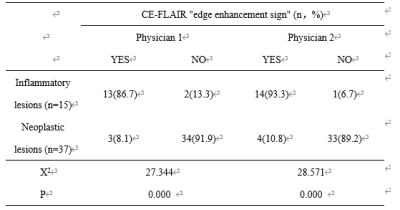
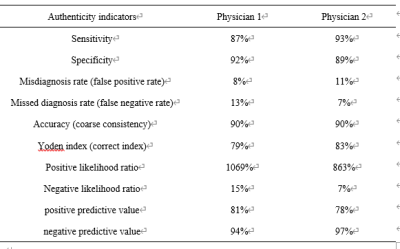
A total of 52 cases of ring-enhancing lesions were collected, including 15 cases of infectious lesions (39.4±22.8 years old, 8 males), 10 cases were confirmed by pathology, and 5 cases were confirmed by clinical follow-up observation. There were 5 cases of brain abscess, 2 cases of tuberculous meningitis, 2 cases of viral meningitis, 5 cases of bacterial meningitis, 1 case of autoimmune encephalitis. In addition, 37 cases of neoplastic lesions (53.6±15.8 years old, 24 males) were confirmed by surgery and pathology. Among them, 9 cases were glioblastoma, 6 cases were schwannomas, and 22 cases were metastases. The typical cases were demonstrated in Figure 1. Table 1 summarized two doctors’ judgments on CE-T2-FLAIR "marginal enhancement sign". Physician 1 judged that 16 cases had CE-FLAIR "marginal enhancement sign", 13 of which were infectious lesions; Physician 2 judged that 14 cases had CE-FALIR "marginal enhancement sign", Of which 8 cases were infectious lesions. Both of them highlighted the its higher diagnosis performance for differentiating the inflammatory lesions and neoplastic lesions (Table 2). In addition, the Kappa value was equal to 0.913 (P = 0.000), which demonstrated the high consistency between the two doctors. CE-T2-FLAIR "marginal enhancement sign" had a statistically significant difference between inflammatory lesions and neoplastic lesions (P<0.05).Discussion
Our results indicated that the infectious lesions were more likely to demonstrate the CE-T2-FLAIR “marginal enhancement sign”. We speculated that this may relate to the phenomenon that the new capillaries of the inflammatory granulation tissue were more included in the edge of the infectious lesion. Specifically, the bacteria stimulate the inflammatory granulation tissue around the lesion and the proliferation of capillaries appears when the inflammatory lesion is in the abscess formation or earlier stage, which limits and repairs to a certain extent. At the same time, the new capillaries and the fibrous tissue will surround the lesion together, limiting the spread of the disease. Due to the good permeability of new capillaries, the contrast agent is easy to leak during enhanced scanning, and T2 FLAIR is more sensitive to low-concentration contrast agents and can show lesions that cannot be displayed on CE-T1WI. The small sample size is the main caveat of this study. Previous studies have found that CE-T2-FLAIR is more sensitive to lesions with low contrast agent concentration and has a higher detection rate [7-8].Conclusion
The CE-T2-FLAIR "marginal enhancement sign" has high sensitivity and specificity for the diagnosis of inflammatory lesions. It can be used as an imaging index for discriminating the inflammatory lesions and neoplastic lesions, providing a reference for their identification and clinical diagnosis[9].Acknowledgements
References
[1]Kolakshyapati M , Hashizume A , Ochi K , et al. Usefulness of Histogram-Profile Analysis in Ring-Enhancing Intracranial Lesions[J]. World Neurosurgery, 2019, 131.
[2] Pino-Lopez L, Wenz H, Böhme J, et al. Contrast-enhanced fat-suppressed FLAIR for the characterization of leptomeningeal inflammation in optic neuritis[J]. Mult Scler, 2019, 25(6): 792-800.
[3] Jeevanandham B, Kalyanpur T, Gupta P, et al. Comparison of post-contrast 3D-T(1)-MPRAGE, 3D-T(1)-SPACE and 3D-T(2)-FLAIR MR images in evaluation of meningeal abnormalities at 3-T MRI[J]. Br J Radiol, 2017, 90(1074): 20160834.
[4] Azad R, Tayal M, Azad S, et al. Qualitative and Quantitative Comparison of Contrast-Enhanced Fluid-Attenuated Inversion Recovery, Magnetization Transfer Spin Echo, and Fat-Saturation T1-Weighted Sequences in Infectious Meningitis[J]. Korean J Radiol, 2017, 18(6): 973-982.
[5] Zhang Y, Sun X, Wu J, et al. Value of MRI enhanced FLAIR sequence examination combined with CSF TNF-α detection in the early diagnosis of neonatal purulent meningitis[J]. Exp Ther Med, 2019, 17(4): 3124-3128.
[6] Robin AB, Craig MH, Timothy K, et al. An overview of meningiomas.Future Oncol, 2018, 14(21): 2161-2177.
[7] Smirniotopoulos J G, Murphy F M, Rushing E J, et al. Patterns of contrast enhancement in the brain and meninges[J]. Radiographics, 2007, 27(2): 525-51.
[8] Lee E K, Lee E J, Kim S, et al. Importance of Contrast-Enhanced Fluid-Attenuated Inversion Recovery Magnetic Resonance Imaging in Various Intracranial Pathologic Conditions[J]. Korean J Radiol, 2016, 17(1): 127-41.
[9] Merino J G, Latour L L, Tso A, et al. Blood-brain barrier disruption after cardiac surgery[J]. AJNR Am J Neuroradiol, 2013, 34(3): 518-23.
Figures