2156
Differential cognitive impairment of lateral ventricle small infarct: Brain atrophy and blood oxygen activity under the cortical layer1Institute of science and technology for Brain-Inspired Intelligence, Shanghai, China, 2Key Laboratory of Computational Neuroscience and Brain-Inspired Intelligence (Fudan University), Ministry of Education, Shanghai, China, 3Human Phenome Institute, Fudan University, Shanghai, China, 4Department of Neurology, The Affiliated Zhongshan Hospital of Fudan University, Shanghai, China, 5Philips Healthcare, Shanghai, China
Synopsis
Most of the lacunar infarcts are small and asymptomatic, while the location and accumulation of multiple lacunar infarctions could cause significant physical and cognitive disabilities. In this study, we explore the association between cognitive impairment and brain atrophy in patients with lateral ventricle infarction and whether there were differences in neuro-radiological features.
Introduction
Lacunar infarcts (LI) and white matter hyperintenses (WMH) considered the results of cerebral small-vessel disease, which often found on MRI in the elderly 1. Both of them are associated with vascular risk factors 2 and impaired cognitive functioning 3. LI and WMH are the primary type of brain lesions is subcortical vascular dementia 4 and are associated with cognitive decline in non-demented elderly 2, 5. Early macroscopic brain loss, measured by serial MRI, has been shown to be a predictor of cognitive decline in Alzheimer Disease (AD) and mild-cognitive impairment 6. Lateral ventricle infarct as the most common type of LI, few studies have focused on lateral ventricle infarct usually causes atrophy in which brain regions. And few studies adjust for shared vascular risk and environmental factors, thus the association between cerebral small-vessel disease and brain atrophy does not necessarily imply a direct relation. Furthermore, few studies have been conducted to calculate blood oxygen activity in patients with lateral ventricle infarction. Due to the lateral ventricle infarction and WMH differ with respect to their cerebral localization and their effect on cognitive performance, we hypothesized that their relation with brain atrophy may also differ. In this present study, we investigate whole-brain morphological differences using voxel-based morphometry (VBM) analysis, and analyze the association among lateral ventricle infarction, brain atrophy and WMH.Materials and methods
Sixty patients (age 30-80 years) with confirmed clinical and MRI diagnosis of acute lateral ventricle infarction were recruited in this voxel-based morphometry and neuropsychological study. MRI acquisition and neuropsychological assessment were conducted within one month of diagnosis. MRI was performed with Philips 3.0T Ingenia MRI system equipped with a 32-channel phased-array head coil at Zhongshan Hospital (Shanghai, China). The protocol included T1-weighted, fMRI, TOF, diffusion tensor imaging and diffusion weighted imaging. The images were acquired as follows: TR = 986ms, TE = 30ms, Matrix =128 x128, slices = 78 slice thickness =2.5mm. Voxel-based morphometry (VBM) was conducted using CAT12, a toolbox of statistical parametric mapping 12. Images were segmented into gray matter, white matter, and cerebrospinal fluid using the standard segmentation module. Rs-fMRI data for computing fALFF and ReHo were preprocessed using a MATLAB toolbox, the Data Processing Assistant for RESTplus V1.21 Basic Edition, which was based on statistical parametric mapping software functions and REST software. Statistical analyses were performed using the SPSS 22.0 for Windows (SPSS Inc., USA) with p<0.05 as the significance criterion. The association among lateral ventricle infarction, brain atrophy and WMH was assessed with analysis of covariance and linear regression analyses. In the multivariate adjusted Cox models, we adjusted for age, gender, PM2.5, water quality, BMI, smoking status and alcohol intake.Results and discussion
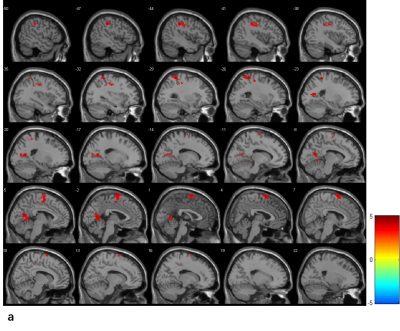
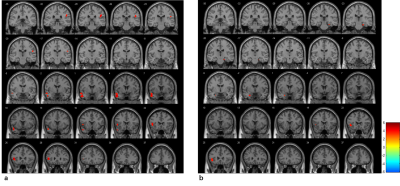
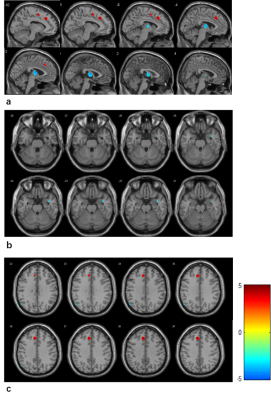
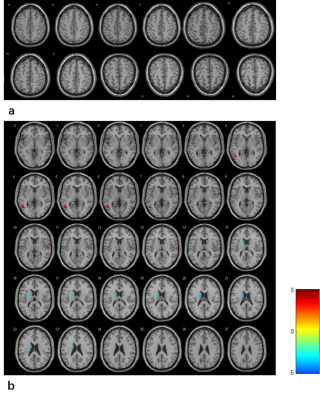
Patients with mild-cognitive impairment (MCI-V) were significantly older than those who without it. In the voxel-based morphometric study, patients with MCI-V in the MMSE group demonstrated more atrophy bilaterally in the thalamus, inter-Hemispheric, medial Dorsal Nucleus and third Ventricle were significantly higher in the MMSE group. Patients with MCI-V in the MoCA group illustrated more bilaterally in the Caudate_L, Extra-Nuclear and Caudate Body. The fALFF of frontal lobes and temporal lobes in patients with MCI-V were higher in the MMSE group, while there was no significant difference in the MoCA group. The ReHO of frontal lobes and temporal lobes in patients with MCI-V were higher in the MMSE group, and the ReHO of parahippocampal gyrus and temporal lobes in patients with MCI-V were higher in the MoCA group. Correlation analysis of MMSE and MoCA scores and grey matter volumes, whiter matter volumes shows that the brain atrophy and cognitive impairment are significantly related to chronic small sub-cortical infarct. We observed that lateral cerebral small infraction is associated with total cerebral atrophy, independent of cortical atrophy. Our findings suggest a differential role for lateral cerebral small infarct and WMH in the development of brain atrophy. In addition, long term exposure to poor living environment is positively associated with lateral cerebral infraction. In summary, in patients with lateral cerebral infarct, lateral cerebral infarction was associated with more total atrophy, independent of the volume of WMH. Furthermore, WMH were associated with more total and sub-cortical brain atrophy.Conclusion
In conclusion, this study represents the association among lateral ventricle small infarction, brain atrophy and WMH. The results indicated a differential role for lateral cerebral small infarct and WMH in the development of brain atrophy. In further study, more subjects will recruit and we will define region of interest and conduct fiber tract analysis.Acknowledgements
This work was supported by ZIB Consortium.References
1. Leeuw FE, Groot JC, Achten E, et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. J Neurol Neurosurg Psychiatry. 2001;70:9-14
2. Longstreth WT, Bernick C, Manolio TA, et al. Lacunar infarcts defined by magnetic resonance imaging of 3,660 elderly people: the Cardiovascular Health Study. Arch Neurol. 1998; 55:1217-1225.
3. Arba F, Quinn T, Hankey GJ, et al. Cerebral small vessel disease, medial temporal lobe atrophy and cognitive status in patients with ischaemic stroke and transient ischaemic attack. European Journal of neurology. 2017;24(2):276-282.
4. Breteler MM, Swieten JC, et al. Cerebral white matter lesions, vascular risk factors, and cognitive function in a population-based study: the Rotterdam Study. Neurology. 1994;44:1246-1252.
5. Pantoni L, Poggrsi A, Inzitrai D. Cognitive decline and dementia related to cerebrovascular diseases: some evidence and concepts. Cerebrovasc Dis. 2009;27(1)191-196.
6.Desmond DW. Cognition and white matter lesions. Cerebrovasc Dis. 2002;13(2):53-57
Figures