2104
MRI-based quantitation of liver fat fraction does not predict the hypertrophy rate in patients with colorectal liver metastases undergoing PVE1Department of Diagnostic and Interventional Radiology, RWTH Aachen University Hospital, Aachen, Germany
Synopsis
There is a substantial clinical need to identify patients who benefit from PVE procedure before undergoing major liver surgery. Elevated liver fat fraction is a frequent finding on pre-procedural MRI based on increasing rates of (non-) alcoholic fatty liver disease as well as chemotherapy-associated steato-hepatitis. Therefore, it was this studys aim to investigate the correlation of MRI-based liver fat fraction on hypertrophy rates after PVE.Including patients with colorectal liver metastases undergoing a single type of portal vein occlusion only there was no correlation found indicating that MRI-based high liver fat fraction should not discourage to perform PVE.
Portal vein embolization (PVE) is used to induce hypertrophy of the future liver remnant (FLR) in patients scheduled for (extensive) hepatectomy, typically for colorectal cancer liver metastases (CRCLM). Fat deposition within the liver is a frequent finding, especially in patients after chemotherapy, and is known to be associated with an impaired liver function and regenerative ability. Since there is a substantial clinical need to identify prognostic factors of patients outcome after PVE we investigated the association between MRI-derived pre-procedural hepatic fat fraction (hFF) on the degree of hypertrophy of the FLR after PVE in patients with CRCLM.
METHODS
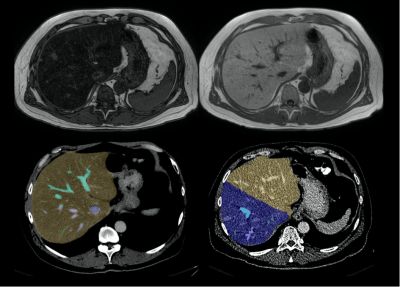
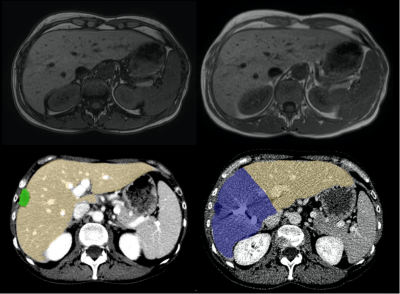
Between 11/2011 and 02/2020, 68 patients (45 males, 23 females, mean age 60 ± 10y) with CRCLM underwent liver MRI, according to a standardized protocol, before PVE. The hepatic fat fraction (hFF) was assessed using regions of interest (ROI) with a diameter of 1.5- 2 cm2 in every segment of the left liver lobe on T1w chemical shift imaging (DUAL FFE) on a 1.5 Tesla MRI (Philips Ingenia). Patients were categorized according to their liver FF as having normal hFF (<5%) or elevated hFF (>5%). Moreover, volumetric liver analysis was performed using a state-of-the-art liver analysis software to calculate total liver volume, FLR percentage, hypertrophy rate and weekly kinetic growth rate on pre-/ and post-interventional imaging. The association of pre-procedural hFF, patient age, gender, initial tumor mass and history of chemotherapy with the degree of liver hypertrophy and FLR growth rates after PVE was investigated using a multiple regression analysis. Correlations were assessed using Spearman test.
RESULTS
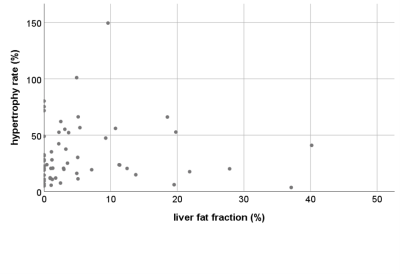
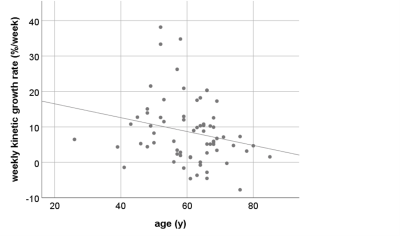
Mean hFF was 6 ± 9% (range 0-40%). Normal hepatic FF was found in 43/68 patients (63%) and increased hFF in 25/68 (37%). Mean hypertrophy and growth rate in patients with normal vs. intermediately increased or high FF were 24 ± 31% vs. 28 ±36% and 9 ± 9% vs. 8 ± 10% (p > 0.05). Spearman test did not show a correlation between hFF and degree of hypertrophy (R = -0.04). Multivariable analysis did not show a correlation between hFF, history of chemotherapy, baseline tumor burden or laterality of primary colorectal cancer.There is a loose inverse correlation between patient age and kinetic growth rate after PVE (R= -0,24; p= 0,04).
DISCUSSION
Portal vein embolization is routinely used to induce growth to the future liver remnant which enables patients with borderline resectable liver metastases to still undergo a potentially life-saving surgical procedure. Patients outcome after PVE is still highly variable. Up to 5% of liver resections are cancelled due to insufficient FLR hypertrophy, another 4% if patients die after surgery mainly due to hepatic failure most likely arising from a small for size syndrome [1; 2]. In conclusion there is a significant clinical need to identify those patients who benefit from the procedure.Respecting increasing rates of alcoholic and non-alcoholic fatty liver disease and risk of chemotherapy-associated steato-hepatitis it was this studys aim to investigate whether MRI-based hepatic fat fraction can be used as a predictor.The finding that there was no association of fat fraction and liver hypertrophy is somewhat counter-intuitive and against our expectation and contradicts a prior report by Barth et al on 45 patients undergoing MRI prior to and after PVE [3]– however, it is in agreement with another study by Geisel et al, on 37 patients [4]. The discrepancy between our findings and those made by Barth et al might be attributable to the fact that in their study, a variety of surgical, interventional, and combined procedures were used for portal vein occlusion. Our study, as well as that by Geisel et al, focused on patients undergoing percutaneous portal vein embolization. A loose inverse correlation was found between patients age and weekly KGR indicating that elderly might have a reduced growth capacity of liver tissue. This seems plausible and in agreement with other studies that found that sarcopenia – as evidenced by a reduced psoas muscle mass – is associated with reduced hypertrophy rates of the FLR after PVE [5].Our study has several limitations. First, our study cohort – although comparable to those of previously published studies on this issue – is still small. We strived to include a homogeneous patient cohort consisting of patients with colorectal liver metastases only undergoing a single type of portal vein occlusion procedure (PVE). Second, using chemical shift imaging for liver fat quantitation does not account for T2* relaxation effects. However, based on pathologic reports, no patient in our cohort showed signs of abnormally high iron deposition in the liver. Hence, we do expect the T2* relaxation effects in our cohort to be only minor.
CONCLUSION
Well over one-third of patients scheduled for PVE exhibit elevated hepatic FF. However, hFF levels are not associated with the degree of hypertrophy that is observable after PVE. An elevated hFF should therefore not be used to discourage PVE procedures in these patients.
Acknowledgements
No acknowledgement found.References
1 van Lienden KP, van den Esschert JW, de Graaf W et al (2013) Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol 36:25-342
2 Isfordink CJ, Samim M, Braat M et al (2017) Portal vein ligation versus portal vein embolization for induction of hypertrophy of the future liver remnant: A systematic review and meta-analysis. Surg Oncol 26:257-2673
3 Barth BK, Fischer MA, Kambakamba P, Lesurtel M, Reiner CS (2016) Liver-fat and liver-function indices derived from Gd-EOB-DTPA-enhanced liver MRI for prediction of future liver remnant growth after portal vein occlusion. Eur J Radiol 85:843-8494
4 Geisel D, Raabe P, Lüdemann L et al (2017) Gd-EOB-DTPA-enhanced MRI for monitoring future liver remnant function after portal vein embolization and extended hemihepatectomy: A prospective trial. Eur Radiol 27:3080-30875
5 Schulze-Hagen M, Truhn D, Duong F et al (2020) Correlation Between Sarcopenia and Growth Rate of the Future Liver Remnant After Portal Vein Embolization in Patients with Colorectal Liver Metastases. Cardiovasc Intervent Radiol 43:875-881
Figures