2101
High resolution of 4D flow MRI with joint 4D flow simulation to optimize magnetic resonance navigation of microrobots at the bifurcation.
Cyril Tous1, Ivan Dimov1, Ning Li1, Simon Lessard1, and Gilles Soulez1
1Radiology, Centre de recherche du Centre hospitalier de l’Université de Montréal, Montreal, QC, Canada
1Radiology, Centre de recherche du Centre hospitalier de l’Université de Montréal, Montreal, QC, Canada
Synopsis
4D flow MRI was used to evaluate flow patterns in 35 and 60 degree one bifurcation PVA phantoms (diameter: 4mm main branch, 3mm branches) with and without resistance in one branch. Multiple spatial resolutions were compared with ink injection and manual measurement for validation. Since computational flow models are frequently used in small vessels, 4D flow was compared with a model. Slow, turbulent flow in the outer side of the bifurcation created eddies where some microrobots get trapped. These eddies were quantitatively and qualitatively characterized with 4D flow. Spatial resolution impacts the accuracy of flow measurement at this scale.
Introduction
Although 4D flow magnetic resonance imaging is reliable for larger blood vessels such as the aorta or inferior vena cava, flow in smaller vessels is usually modeled with computational fluid dynamics due to the limited spatial resolution of MRI. Successful flow imaging in small vessels can validate and improve computational models, allowing better selectivity of transarterial chemoembolization and eventually navigation of drug-loaded microrobots in the bloodstream. Here, changes in net flow, vessel bifurcation angle and flow resistance in branches of phantoms were investigated with 4D flow and computational models.Methods
CT angiograms of the proper hepatic artery in 19 patients yielded a minimum angle of 35° and average angle of 60° at the first bifurcation. Since polyinyl alcohol (PVA) can reproduce inner friction of blood vessels1, we designed one-bifurcation PVA phantoms with internal diameter of 4mm in the main branch and 3 mm in the branches. The flow ratio between the left and right lobe of a liver is 1 to 2, respectively. Therefore, resistance with smaller tubes was added to the left branch of the phantom. The phantom was placed parallel to B0 in a 3T MRI scanner and perfused with 25°C water by a cardiac pump set at 60 beats per minute and 14 mL stroke volume. Continuous infusion at 0.2 ml/sec through a deflated angioplasty catheter placed in the main branch yielded a 1.2ml/s pulsatile flow. The system was connected to a bypass with a pressure transducer, recording a pressure of 120/60 mmHg. The triggers (5V, Pulse length = 10 ms, Phase position: 200ms before peak systole) were automatically generated based on the obtained pressure waveform to synchronize the 4D flow (Siemens WIP785B, parameters in Table 1) and cine phase sequences (TR=100.64ms, TE=3.61ms, voxel=0.4x0.4x3.7mm3, slice=1, FOV=200x200, VENC=40cm/s, TA=1min). Analysis was performed using Argus, WIP 4D flow demonstrator (v2.4, Siemens) and Comsol Multiphysics.Results
According to the acquisition parameters (Table 1) and the manual measured flow (Table 2), our model simulates a laminar flow in the main branch with a peak velocity between 9.5 and 12 cm/s. Simulated eddies with turbulent flow inferior to 3 cm/s appear in the outer angles of the bifurcation. A flow channel forms in the inner half of the branches where microrobots have enough hydrodynamic drag (velocity>8cm/s) to cross the bifurcation. This is confirmed by visually tracking with a camera the injected aggregates of microrobots (n=50) through the bifurcation. Ink injected from the catheter shows low flow areas corresponding to the eddies (Figure 3-A). On the other hand, the 4D flow at 0.4mm2 in plane resolution shows absence of streamlines in the eddies (Figure3-D) and a reduction of flow from 9cm/s to 4cm/s in the inner bifurcation angle (cross section 71 and 72, Figure 4). The average velocity measured in the left branch without and with resistance decreased from 6.50 cm/s to 4.16cm/s. In the opposite branch the flow velocity increased from 8.71cm/s to 9.29cm/s. The flow velocity in the main branch changed from 13.05cm/s to 11.28cm/s with resistance. The change of flow distribution is noticeable in Figure 4-D. When resistance occurs in the left branch (B1), the flow decreases from 4cm/s (Figure 4-C) )to 1cm/s (Figure 4-D)Discussion
A 4D flow acquisition at 0.2mm2 in plane resolution reaches the noise floor which overestimates the flow velocity. Therefore 4D flow at 0.4mm2 resolution is appropriate to characterise flow patterns while at 1.5mm2 resolution it was not possible to obtain 4D flow information in 3mm diameter branches. The slight phase difference of measured velocity in Figure 4 is related to the attributed number of the cross section while the significant flow loss characterizes the eddies and the outer bifurcation flow decreases in these cross sections. We demonstrated that with appropriate triggering in an in vitro experiment simulating in vivo condition it is possible to perform 4D flow and measure complex flow patterns and resistance in order to optimize 4D modelling.Conclusion
4D Flow can provide micro fluid dynamic information (vortices, eddies, inner angle of the bifurcation) to validate computational models and explain microrobot movement. The spatial resolution and other acquisition parameters require further optimization.Acknowledgements
Canadian Institutes of Health Research
Siemens Healthineers, Canada
Transmedtech, Canada
References
No reference found.Figures
Figure 1) Acquisition parameters for high resolution 4D flow (1.5mm², 0.75mm², 0.4mm², 0.2mm² in plane resolution using interpolation) in one bifurcation PVA phantoms.
Figure 2) Manual measurement of the flow rate in the branches of the 35° and 60°phantoms with and without resistance.
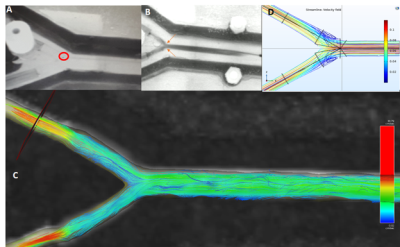
Figure 3) A microrobot (A, red circle) in the 60 degree bifurcation PVA phantom stuck in an eddie visualized using ink (B, orange arrows) and 4D flow (C) (0.4x0.4mm2 in plane resolution). The eddies were simulated with streamlines (D).
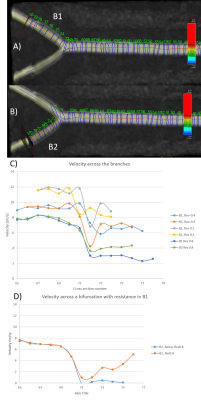
Figure 4) Measurement of the flow velocity according to the resolution of acquisition and the cross section without and with resistance in the branch (B1, left).