2074
Multi-VENC 4D flow MRI demonstrates pulmonary stenosis and arterial-pulmonary collateral in congenital conotruncal anomaly1Tokyo Women's Medical University, Tokyo, Japan, 2Philips Japan, Tokyo, Japan
Synopsis
We propose a free-breathing 4D flow sequence with echo-planar imaging (EPI) and rapid reconstruction to facilitate clinical use. Pulmonary stenosis or atresia is a common anatomic component of congenital conotruncal anomaly. Multi-VENC 4D flow MRI with EPI can simultaneously visualize the pulmonary artery stenosis and associated collaterals of slow flow formed by peripheral arteries. Consequently, all sources of pulmonary blood supply and of the size and morphology of the pulmonary arteries can be completely delineated.
Introduction
Pulmonary stenosis or atresia is a common anatomic component of congenital conotruncal anomaly. The central pulmonary arteries may be hypoplastic, discontinuous, or abscent. Therefore, the pulmonary vascular bed may be supplied with blood flow from antegrade flow through the pulmonary valve, arterial-pulmonary collaterals, and surgically placed shunts. Complete delineation of all sources of pulmonary blood supply and of the size and morphology of the pulmonary arteries is essential to patient management (1). We propose a free-breathing 4D flow sequence with echo-planar imaging (EPI) and rapid reconstruction to facilitate clinical use (2). We investigate the ability of multi-VENC 4D flow with EPI for detection of arterial-pulmonary collaterals in adults conotruncal anomaly after bi-ventricular repair.Materials and Methods
4D flow data with 3.0 tesla imager (Ingenia 3T CX, Philips Healthcare) for consecutive 165 patients with conotruncal anomaly [age range, 18-63 years; tetralogy of Fallot (TOF), 116; complete transposition of great arteries (TGA), 26; corrected TGA (cTGA), 23] was analyzed. Afree breathing and flow-sensitive 3D gradient sequence with EPI was used as 4D flow. The first 110 patients were set to one of the VENC 150 or 200 cm/s, and the second half 55 patients were set to VENC 50-70 cm/s in addition to the VENC 150 or 200 cm/s. Immediately after the acquisition, rotational reconstructed images including the whole heart and great vessels were created. The presence or absence of pulmonary artery stenosis >70% of the main or the bilateral PA (PA stenosis), and arterial-pulmonary collaterals were evaluated.Results & Discussion
Of the first 110 patients scanned using only VENC 150 or 200 cm/s, 15 patients had PA stenosis (14%). One of them found to have arterial-pulmonary collaterals (7%). Of the following 55 patients scanned using multi-VENC, 8 patients had PA stenosis (15%). Six of them had arterial-pulmonary collaterals on the 4D flow images with VENC 50-70 cm/s (75%). Multi-VENC 4D flow had a significantly higher detection rate of arterial-pulmonary collaterals in PA stenosis than single-VENC 4D flow. Collateral donor arteries were the bronchial artery in 3 cases, the internal thoracic artery in 3 cases, the subclavian artery in 2 cases, and the intercostal artery in 2 cases. Non-contrast multi-VENC 4D flow MRI with EPI can improve velocity resolution, reduce noise, and scan time (3 minutes). A single optimal VENC setting might be inappropriate in difficult situations of complex flow patterns or vascular territories, such as arteriovenous malformations or congenital heart disease with dual arterial and venous blood supply (blue arrow, supplementary material). Furthermore, non-contrast dual VENC 4D flow MRI with EPI is feasible as a screening tool in patients with renal dysfunction or contrast allergy.Conclusion
Multi-VENC 4D flow MRI with EPI can simultaneously visualize the pulmonary artery stenosis and associated collaterals of slow flow formed by peripheral arteries. Consequently, all sources of pulmonary blood supply and of the size and morphology of the pulmonary arteries can be completely delineated.Acknowledgements
This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI (19K08209).References
1. Geva T, Greil GF, Marshall AC, et al. Gadolinium-enhanced 3-dimensional magnetic resonance angiography of pulmonary blood supply in patients with complex pulmonary stenosis or atresia: comparison with X-ray angiography. Circulation 2002; 106: 473-478.
2. Shiina Y, Inai K, Miyazaki S, Nagao M. Aortic vorticity, helicity, and aortopathy in adults patients with tetralogy of Fallot: pilot study using four-dimensional flow magnetic resonance images. Pediatric Cardiology 2020 https://doi.org/10.1007//s00246-020-02466-0.
Figures
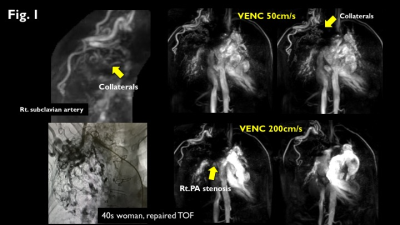
Figure 1.
50s woman with repaired TOF. VENC 50cm/s images can emphasise slow venous flow like collaterals without contrast medium (upper row). Arterial-pulmonary collaterals from the right subclavian artery were detectedas well as angiography (left lower). VENC 200cm/s images show severe stenosis at the proximal right PA (lower row).
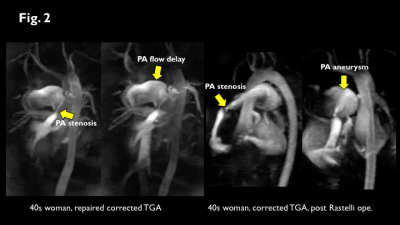
Figure 2.
4D flow with VENC 200cm/s shows typical flow pattern of PA stenosis and aneurysm.