2063
TKE measurement based on 4D Flow MRI can predict distal aortic expansion after artificial blood vessel replacement for type A aortic dissection1Nippon Medical School Hospital, Tokyoto Bunkyoku, Japan
Synopsis
To investigate whether turbulent kinetic energy measurement around anastomosis can be used as a predictor for residual aortic expansion after aortic replacement for type A aortic dissection. The TKEpeak of AoR group was significantly higher than those of volunteers (15.12 ± 7.06 [3.51–28.38] vs. 4.50 ± 1.64 [2.57–8.13] mJ, p < 0.001). There was a strong correlation between the annual expansion rate and distal TKEpeak (R²=0.818).
Introduntion
Recently, the long-term outcome for type A aortic dissection (AAD) has been more discussed thanks to the improvement of short-term mortality after the surgical treatment, aortic replacement (AoR) (1). According to previous reports, 40% of AAD after AoR exhibit distal aortic expansion within 5 years, some of whom require reoperation (2, 3). If we can predict morphological changes in these patients, the management including surgical options would be improved.It is generally accepted that the abnormal vessel wall stress via turbulent flow induces the aortic expansion (4). In previous reports, wall shear stress (WSS) has been mainly used as the marker of this phenomenon (4). However, its value calculated from 4D Flow MRI is not accurate because it is sensitive to several factors such as spatial resolution, vessel wall motion, and the boundary condition of the vessel wall. To overcome these drawbacks, we expected that turbulent kinetic energy (TKE) can be used as a surrogate marker for abnormal vessel wall stress. TKE is calculated from the signal drop induced by the combination with bipolar gradient and turbulence on magnitude images of 4D Flow MRI. Its concept is not the same but similar to diffusion-weighted images. One of the advantages of TKE is that it is robust to the changes in spatial resolution. The other is that we can measure its value with enough volume of interest (VOI) (e.g. the whole intravascular regions of ascending aorta). Its utility has been already validated in a few previous reports (5, 6).
The purpose of this study was to investigate whether TKE around the anastomosis can be used as a predictor for residual aortic expansion after AoR for AAD.
Method
Nippon Medical School Hospital’s ethics committee approved this observational study (30-08-986). Informed consent was obtained from all subjects.Subjects;
From May 2018 to January 2020, we recruited 13 patients (56.5±12.3 years old, 10 males) who had undergone AoR for AAD and 9 normal volunteers (30.9±3.0 years old, 6 males).
Imaging and reconstruction;
4D Flow MRI using a 3.0-T MRI unit (Achieva; Philips Healthcare) was performed. The parameters were as follows; TR/TE, ≈ 4.0 / 2.7ms; FA, 11 degrees; voxel resolution, 1.7*1.7*2.0-2.0*2.0*2.5mm; multi-VENC acquisition, 50–100–300 cm/s; heart phase, 15–21 depending on heart rate; prospective triggering; k-t PCA acceleration factor, 5–7; free breath acquisition; and acquisition time 8–12 min. TKE was calculated from the magnitude images of multi-VENC data combined with Bayesian estimation by using offline reconstruction software (CRECON, Gyro Tools, Zurich, Switzerland).
Analysis;
GT Flow (GyroTools, Zurich, Switzerland) was used for TKE quantification. The VOI from left ventricular to aortic arch was drawn semi-automatically based on phase-contrast MRA imaging. TKEphase is calculated as the sum of entire VOI at each cardiac phase. TKEpeak was the highest TKEphase in the whole cardiac phase.
Statistical analysis;
First, TKEpeak was compared between AoR group and volunteers by using Mann-Whitney U-test. Second, the TKE elevation on the caudal side from the distal end of the graft was defined as the distal TKEpeak. The annual expansion rate on the distal side of the graft was calculated for patients followed up for 6 months or more after surgery. We investigated the correlation between the annual expansion rate on the distal side of the graft and distal TKEpeak. In all analyses, p < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 19.0.0 (IBM Corporation, Armonk, NY, USA).
Result
Out of 13 patients, 1 patient was excluded because an electrocardiogram could not be acquired because of arrhythmia. Hence, we evaluated 12 patients (59.5 ± 12.2 years old, 9 males) and 9 normal volunteers (30.9 ± 3.0 years old, 6 males). All of the acquired data was listed in table 1. The representative case was illustrated in figure 1 and 2. The TKEpeak of AoR group was significantly higher than those of volunteers (15.12 ± 7.06 [3.51–28.38] vs. 4.50 ± 1.64 [2.57–8.13] mJ, p < 0.001). There was a strong correlation between the annual expansion rate of the distal aorta of the anastomosis and distal TKEpeak (R²=0.818) (figure 3).Discussion
The current study revealed that accelerated jet flow occurs at the distal side of anastomosis, leading to the elevation of TKE. Its elevation is highly correlated to the annual expansion rate of residual aortic expansion. Based on the result, we assume that TKE accurately reflects the “turbulence” of the aorta. This turbulence causes abnormal WSS which inducing distal aortic expansion. This hypothesis is based on several previous reports. First, TKE correlates wall shear stress in the simulation study (7). If this correlation maintains in vivo, TKE is more useful than WSS because it is robust to spatial resolution and enough VOI can be drawn for the measurement. Second, it is suggested that TKE elevation of AS correlates with aortic expansion (5). The limitation is that we only focused on TKE in small patients. Therefore, further studies including the comprehensive analysis of other flow parameters such as WSS in a larger cohort.Conclusion
After AoR for AAD, TKE calculated from 4D Flow MRI is significantly increased than volunteers. TKE can be used to predict expansion on the distal side of the anastomosis.Acknowledgements
No acknowledgement found.References
1.Emily Pan, et al. Low rate of reoperations after acute type A aortic dissection repair from The Nordic Consortium Registry. J Thorac Cardiovasc Surg 2018;156: 939-948. 2.Claudio F Russo, et al. Italian multicentre study on type A acute aortic dissection: a 33-year follow-up. European Journal of Cardio-Thoracic Surgery 2015:125-131. 3.Zhengjun Wang, et al. Long-term outcomes of survival and freedom from reoperation on the aortic root or valve after surgery for acute ascending aorta dissection. The Journal of Thoracic and Cardiovascular Surgery 2014:2117-2122. 4. Garcia J, et al. The Role of Imaging of Flow Patterns by 4D Flow MRI in Aortic Stenosis. JACC Cardiovasc Imaging. 2019;12(2):252–266. 5. Christian Binter, et al. Turbulent Kinetic Energy Assessed by Multipoint 4-Dimensional Flow Magnetic Resonance Imaging Provides Additional Information Relative to Echocardiography for the Determination of Aortic Stenosis Severity. Circ Cardiovasc Imaging 2017; 10 6. Kotomi Iwata, et al. Four-dimensional flow magnetic resonance imaging reveals the reduction in turbulent kinetic energy after percutaneous transluminal septal myocardial ablation in hypertrophic obstructive cardiomyopathy. Eur Heart J 2019 7. Magnus Ziegler, et al. Assessment of turbulent flow effects on the vessel wall using four-dimensional flow MRI. Magn Reson Med. 2017Figures
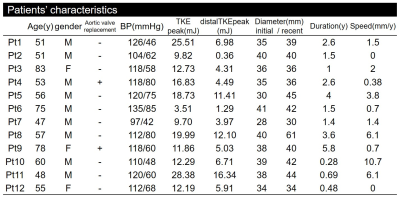
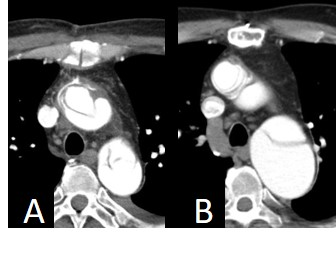
Figure 1. 58-years-old male after ascending aorta replacement.
A: Contrast-enhanced CT image immediately after surgery
B: Contrast-enhanced CT 4 years after surgery, which shows an increase in blood vessel diameter on the distal side of the replaced aorta is observed at a rate of 6.1 mm per year.
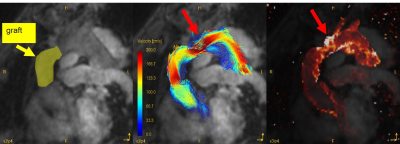
Figure 2. The same patient as figure 1
A: The yellow part indicates the graft.
B: This velocity image shows jet flow on the distal side of the graft (red arrow).
C: TKE image map shows that TKEpeak is increased especially on the distal side of the anastomosis of the graft (red arrow), which corresponds to the part where the flow velocity is increased.
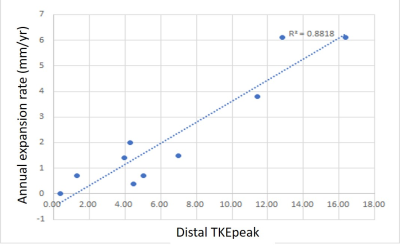
Figure 3. The correlation between the annual expansion rate or the residual aorta and distal TKEpeak.
A strong correlation was observed