2062
Decreased sciatic nerve fractional anisotropy in diabetes and prediabetes associated with lower and upper limb function impairment1Heidelberg University Hospital, Heidelberg, Germany
Synopsis
Nerve damage in distal polyneuropathy first becomes clinically apparent in in the legs and later in hands and arms. Previous studies could show, however, that peripheral nerve lesions in the leg predominate in the thigh and that upper limb nerve function can be impaired in early stages of the disease. We show that a decrease in sciatic nerve fractional anisotropy is associated with impaired nerve function in both upper and lower limbs for patients with diabetes and patients with prediabetes. Our findings therefore suggest that structural nerve damage in diabetic polyneuropathy already occurs at early, subclinical stages of the disease.
Purpose
Distal symmetric polyneuropathy (DN) is one of the most common and severe chronic complications of diabetes mellitus. While it is generally assumed that nerve damage in DN begins in the lower legs and progresses to hands and arms at later stages, recent studies revealed that nerve lesions in the leg predominate more proximally at the main sciatic nerve level,1,2 and that, in arms, nerve functions can be impaired at early stages of DN.3,4 The purpose of this study was to evaluate if sciatic nerve fractional anisotropy (FA) as a measure for structural nerve integrity would serve as a surrogate marker for functional impairment of both upper and lower limbs in patients with diabetes and prediabetes.Methods
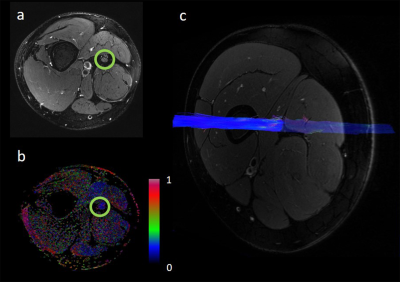
We performed high-resolution magnetic resonance neurography of the right thigh in a 3.0 Tesla MR scanner (MAGNETOM TIM-TRIO, Siemens) in 71 patients with diabetes, 11 patients with prediabetes and 25 age-matched control participants with a T2-weighted turbo spin echo 2D sequence with spectral fat saturation (TR = 5970ms, TE = 55ms, FOV = 160x160mm2, matrix size = 512x512, voxel size = 0.3x0.3x4mm3, 24 slices; see also Fig. 1a) and diffusion tensor imaging using an axial fat-suppressed, diffusion-weighted 2-dimensional echo-planar sequence (TR = 5100ms, TE = 92.8ms, b = 0 and 1000 s/mm2, directions = 20, FOV = 160x160 mm2, matrix size = 128x128, slice thickness = 4mm, voxel size = 1.3x1.3x4mm3, 3 averages, 24 slices, 1512 acquired images; see also Fig. 1b-c). Nerve segmentation and analysis was performed with Nordic BRAINEX and Matlab v7.14.0.0739. We further acquired tibial, peroneal, and sural nerve conduction velocities and compound motor action potentials of the right leg as well as the Purdue Pegboard Test to measure hand dexterity and fine motor skills.Results
The average FA of the sciatic nerve was positively correlated with peroneal and tibial nerve conduction velocity (p<0.001, r=0.56 and p<0.001, r=0.62, respectively), and peroneal and tibial nerve compound motor action potentials (p<0.001, r=0.63 and p<0.001, r=0.62, respectively) in all patients with diabetes. Hand function correlated positively with sciatic nerve FA in patients with diabetes (p<0.001, r=0.52), prediabetes (p<0.001, r=0.76) and in controls (p=0.007, r=0.79).Conclusion
The fractional anisotropy of the sciatic nerve as a marker for the nerve’s structural integrity is associated with a decreased nerve conduction velocity and a decreased hand function in both patients with diabetes and prediabetes. Our results indicate that nerve damage in diabetes affects the entire peripheral nervous system at early stages, and, that MRN fractional anisotropy in diabetes and prediabetes may serve as a surrogate parameter for functional and electrophysiological evaluations of the upper and lower limbs. The findings further suggest that structural nerve damage related to functional impairment occurs prior to or at very early stages of type 2 diabetes and is not, as mostly assumed, a late complication of this disease.Acknowledgements
The German research council (DFG, SFB 1158) provided financial support of this study.References
1. Pham M et al., Ann Neurol 2015;78(6):939-948
2. Jende JM et al., Ann Neurol 2018;83(3):588-598
3. Kopf S et al., Diabetes Res Clin Pract 2018;146:191-201
4. Yang CJ et al., J Diabetes Ingestig 2018;9:179-185