2059
Can Diffusion Kurtosis Imaging and 3D-Arterial Spin Labeling perfusion imaging improve the diagnostic accuracy of Binswanger's Disease?1Department of Medical Imaging, Shandong Provincial Qianfishan Hospital, The First Hospital Affiliated with Shandong First Medical University, Jinan, China, 2Shandong First Medical University, Taian, China, 3GE Healthcare, MR Research China, Beijing, China
Synopsis
This study aimed to investigate whether the combined 3D-arterial spin labeling (3D-ASL) and diffusion kurtosis imaging (DKI) can distinguish Binswanger’s disease (BD) patients from healthy subjects. 35 BD patients and 33 age/gender-matched controls were scanned in DKI and ASL at 3T. Compared with healthy subjects, significant alterations were found in almost all DKI & ASL relevant parameters on the major lesions and partial non-lesion regions of BD. With these findings, we thus proved that the combined DKI and 3D-ASL can be effectively tools exploring pathophysiological mechanisms and performing robust diagnostic accuracy for BD patients.
Introduction
Binswanger’s disease (BD), as a major subtype of subcortical vascular dementia, has a dramatically increased prevalence rate in recent years1. While the pathological features (the impairment of blood-brain barrier and white matter nerve fibers) and MRI features (leukoaraiosis, multiple infarction and atrophy)2,3 can help for clinical diagnosis of BD, a consensus on BD diagnostic criteria is still lacking, which thus leads to low diagnostic accuracy in clinic.Diffusion kurtosis imaging (DKI) with a comprehensive set of diffusion and kurtosis related parameters, has been reported to be sensitive in monitoring age-related white matter (WM) changes in elderly patients with leukoaraiosis4. Meanwhile, pseudo-continuous 3D-arterial spin labeling (3D-ASL) is also proposed to monitor the changes in cerebral blood flow (CBF) of leukoaraiosis effectively5. With these features, we assumed that both techniques have potential in the diagnosis of BD patients. Therefore, in this study, the feasibility of combined DKI and ASL in the accurate clinical diagnosis of BD has been investigated.
Material and Methods
Subjects35 patients (23 men, 72.2±6.6 years), clinically confirmed with BD diseases, and 33 age/gender-matched healthy subjects (13 men, 70.6±6.8 years) were recruited in this study.
MRI experiment
All MR experiments were performed at 3.0 Tesla (MR750, GE Healthcare, USA) using an 8-channel head phased array coil. 3D high resolution T1-weighted anatomical imaging (BRAVO), DKI and ASL imaging were performed on each participant.
For DKI scanning, the scan parameters were of TR=2000ms, TE=72.20ms, matrix=256×256, slice thickness=5mm, slice spacing=1.5mm, FOV=260×260mm. Five b values (400, 800, 1200, 1600 and 2000s/mm2) as well as 15 directions at each b value were used.
For 3D-ASL perfusion imaging, the following scan parameters were used, including TR/TE, 4632ms/10.54ms, matrix=128×128, slice thickness=4mm, FOV=240×240mm, and post-labeling delay time=1525ms).
The total scan time was 14 minutes.
Data analysis
Multiple DKI-derived parametric mapping, i.e., FA, MD, Da, Dr, FAk, Mk, Ka, and Kr maps, and 3D-ASL derived CBF mapping were obtained, respectively, using vendor-provided post-processing software on AW4.6 workstation (GE, USA).
Multiple cerebral regions of interest (ROIs) were manually selected twice by two senior radiologists (Fig.1) based on BRAVO and T2W imaging (b=0 s/mm2), including the genu and splenium of the corpus callosum (GCC, SCC), frontal, parietal, and temporal WM (FWM, PWM, TWM) and lateral ventricle around frontal and occipital WM (BV-FWM, BV-OWM), caudate nucleus (Cau), thalamus (Tha), and hippocampus (Hip). The selected ROIs were copied on DKI/ASL parametric maps, and the average values over two measurements were included for further analysis. All ROIs are divided into three groups including lesions of BD (L-BD), non-lesion of BD (N-BD) and normal control (NC), and the N-BD refers to the normal region adjacent to L-BD on the same side and NC was obtained in the healthy subjects.
Statistic analysis
In Graphpad prism software, one-way analysis of variance (ANOVA) followed by post-hoc analysis was first used to assess the differences of each DKI parametric values in each ROIs among three groups. The comparisons of DKI/ASL parameters between the left and right hemispheric ROIs were performed using the paired-samples t-test, and parameter comparisons between N-BD and NC shall use the single-sample t-test. Receiver operating characteristic (ROC) curve of each parameter was analyzed to compare their diagnostic value in differentiating BD from healthy subjects. P < 0.05 was considered statistical significance.
Results
As shown in Fig.2, compared with healthy subjects, significantly declined values were found in FA, FAk, MK, Ka, Kr, and CBF on all lesions of L-BD (FWM, PWM, BV-FWM, BV-OWM) in BD(p < 0.05). In contrast, notably increased patterns were observed in MD, Da, and Dr on these regions (p < 0.05).For N-BD, except for decreased CBF values, significant changes, similar to L-BD, were shown in almost all DKI parameters of the GCC, SCC and TWM. Partial DKI parameters (e.g.,FA, MD, Da, Dr, Ka) of FWM, BV-FWM, BV-OWM, right Cau, Tha and right Hip have also shown significant changes similar to L-BD (Fig.2).
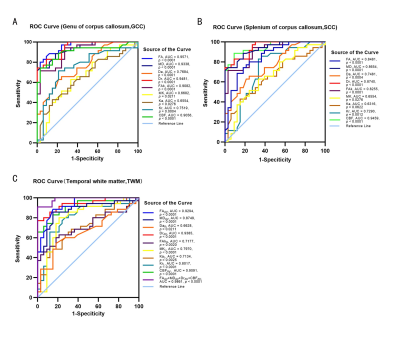
Using ROC analysis, AUC curves identified FA in the GCC (Fig.3.A), CBF in the SCC (Fig.3.B), as well as the combined FA, MD, Dr, and CBF in the TWM (Fig.3.C) indicated high accuracy (AUC values of 0.957, 0.946, and 0.986 respectively) in distinguishing BD patients from healthy controls.
Discussion and Conclusions
This study has investigated whether combined DKI and 3D-ASL can distinguish BD patients from healthy subjects. The significant differences were found in all DKI and ASL parameters between L-BD and NC, and partial DKI parameters of N-BD have also shown significant changes similar to L-BD. ROC analysis showed that FA in GCC, CBF in SCC, and the combination of FA/MD/Dr/CBF in TWM were all highly accurate in distinguishing BD from healthy subjects. These results may indicate that there are serious cerebral circulation disorders and notably damaging in the hydrophobic cell membrane and myelin sheath not only in the L-BD but also in partial N-BD.In conclusion, both DKI and 3D-ASL derived parameters have demonstrated great sensibilities in detecting the alterations of microstructures in L-BD and N-BD. Among these, the DKI parameters of FA, MD, Dr, and Kr and ASL parameter of CBF have performed robust diagnostic accuracy, indicated by high AUC values, and can thus be considered effective biomarkers for BD patients diagnosis in clinic.
Acknowledgements
No acknowledgement found.References
- Rosenberg, G. A. Binswanger's disease: biomarkers in the inflammatory form of vascular cognitive impairment and dementia. Journal of neurochemistry 144, 634-643, doi:10.1111/jnc.14218 (2018).
- Caplan, L. R. & Schoene, W. C. Clinical features of subcortical arteriosclerotic encephalopathy (Binswanger disease). Neurology 28, 1206-1215, doi:10.1212/wnl.28.12.1206 (1978).
- Akiguchi, I. et al. MRI features of Binswanger's disease predict prognosis and associated pathology. Annals of clinical and translational neurology 1, 813-821, doi:10.1002/acn3.123 (2014).
- Xu, S. et al. Assessment of severity of leukoaraiosis: a diffusional kurtosis imaging study. Clinical imaging 40, 732-738, doi:10.1016/j.clinimag.2016.02.018 (2016).
- Zhong, G. et al. Better Correlation of Cognitive Function to White Matter Integrity than to Blood Supply in Subjects with Leukoaraiosis. Frontiers in aging neuroscience 9, 185, doi:10.3389/fnagi.2017.00185 (2017).
Figures
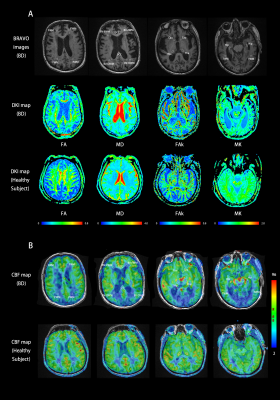

Figure. 2 Comparison of DKI measurements among the three groups and CBF between the different brain regions corresponded in BD and control groups.
Note: L-BD, lesions of BD; N-BD, non-lesions of BD; NC, normal controls; L/R, the left/right-hemispheric side; AV, average of bilateral ROI measurements;GCC/SCC, genu and splenium of the corpus callosum; FWM/PWM/TWM, frontal, parietal, and temporal WM; BV-FWM/BV-OWM, lateral ventricle around frontal and occipital WM; Cau, caudate nucleus; Tha, thalamus; Hip, hippocampus. Significant difference: *p < 0.05; **p <0.001; ***p < 0.0001.