1903
Comparing compressed sensing Breath-hold 3D MR cholangiopancreatography with two parallel imaging MRCP strategies1Radiology, Union Hospital, School of Medical Technology and Engineering, Fujian Medical University, Fuzhou, China, 2Diagnostic imaging, Siemens Healthcare, Shanghai, China., Shanghai, China, 3MR application, Siemens Healthineers Ltd,Guangzhou,China, guangzhou, China
Synopsis
The overall imaging quality of BH CS-MRCP, BH-MRCP and NT MRCP protocols were not significant different. Both the two breath-hold approaches were considering the time-saving advantages without deterioration of image quality. Compared with BH CS-MRCP, BH-MRCP yielded significantly better visualization of the segment 2 and 3 branch of the intrahepatic duct, and performed better consistency in main pancreatic duct and common bile duct morphology. Therefore, BH-MRCP in terms of superior visualization and morphological consistency can be recommended to improve workflow and diagnostic efficacy, and be preferred for patients with irregular breathing pattern.
Introduction
Currently, MRCP techniques typically are performed using respiratory-triggered or navigator-gated three-dimensional (3D) T2-weighted turbo spin echo (TSE)-based sequences, which require 3-6 minutes of acquisition time (1). The main drawback of this method is the long acquisition time leads to image blurring and motion artifacts, particularly in patients with irregular breathing patterns, which could preclude image interpretation. The utility of breath-hold 2D sequence is limited in clinical practice mainly due to lower spatial resolution and no capability for 3D reconstructions (2). Therefore, accelerated parallel imaging (PI) technique have been applied to shorten the acquisition time of 3D MRCP, which significantly reduced imaging time within a single breath-hold (3). A recent approach, compressed sensing (CS), can further increase the acceleration factor of MR acquisition by integrating 3 conditions including sparsity, incoherent sampling and iterative reconstruction algorithm (4). Several recent studies demonstrated CS technique feasible with comparable results to conventional MRCP sequences at 1.5 and 3 T, adopting either CS BH protocol or CS navigator triggered (NT) protocol. However, few literatures studied whether BH MRCP images with high undersampling factors are consistent with those acquired by standard NT-MRCP. Thus, the objective of the present study is to evaluate the image quality and image consistency between BH-MRCP and BH CS-MRCP in patients with suspected pancreaticobiliary diseases, compared with conventional NT-MRCP.Materials and methods:
From April 2020 to September 2020, a total number of 109 patients underwent NT 3D-MRCP, BH-MRCP and BH CS-MRCP were prospectively enrolled in this study. All MR examinations were performed on a 3T MR scanner (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) using an 18-channel body matrix coil combined with a 32-channel spine matrix coil. Patients were asked to fast for at least 4 hours prior to the examination. No spasmolytic drug was administered. The application of a negative oral contrast agent was administered to suppress fluid signal in the stomach and duodenum before the examination unless a contraindication. Volumetric 3D MRCP sequences consisted of NT-MRCP, BH-MRCP, BH-CS MRCP were performed in all patients. Other protocols were also acquired with the standard clinical protocol: T2-weighted axial and coronal sequences with ultra fast spin echo, diffusion-weighted axial sequence, T1-weighted 3D gradient echo before and after gadolinium. These sequences were not used for the data analysis. The conventional 3D MRCP protocol in standard coronal orientation using a sampling perfection with application optimized contrasts using different flip angle evolutions (SPACE) sequence were performed first, and the two BH protocols were followed in a random order. The parameters for MRCP imaging are summarized in Table 1. The Friedman test was performed to compare quantitative values, image acquisition time, the presence of artifacts, overall image quality, and duct visualization among the three protocols. A P-value of less than 0.05 was taken to indicate a significant difference. Additionally, we compared BH-MRCP and BH-CS MRCP with NT-MRCP in morphological consistency of main pancreatic duct and common bile duct (CBD) based on overall image quality score of = 4.Results:
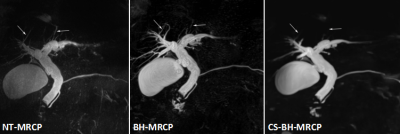
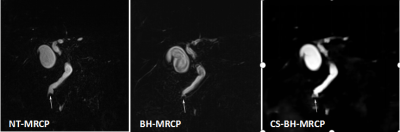
Three MRCP methods were successfully performed in all the patients. Mean acquisition times were 147.2±33.31 s for NT-MRCP, 18 s for BH-MRCP, and 17 s for BH-CS MRCP. Quantitative data are summarized in Table 2. The contrast ratio, SNR and CNR of the CBD were significantly higher for BH-CS MRCP than those for NT-MRCP and BH-MRCP images (0.97±0.02 vs 0.91±0.03 and 0.92±0.02, P<0.001; 12.61±8.34 vs 8.04±4.17 and 7.46±3.51, P<0.001; 17.73±11.73 vs 11.08±5.71 and 10.21±4.66, P<0.001), respectively. However, there were no statistically significant differences between NT-MRCP and BH-MRCP in quantitative image analysis. Representative case is shown in Fig.1. Qualitative results are summarized in Table 3. Overall image quality did not differ significantly among the three sequences: mean scores were 3.44 for NT-MRCP, 3.69 for BH-MRCP, and 3.57 for BH-CS MRCP. Qualitative score for artifacts was significantly higher on BH-CS-MRCP (3.91±0.32) than on NT-MRCP and BH-MRCP (3.58±0.66, 3.41±0.61, respectively, P = 0.001, <0.001). In contrast, segment 2 or 3 branch and main pancreatic duct visualization were significantly better with BH-MRCP than with BH-CS-MRCP and NT-MRCP (p<0.001).Conclusions:
In conclusion, the overall imaging quality of the three MRCP protocols were not significant different. Both the two breath-hold approaches were considering the time-saving advantages without deterioration of image quality. BH CS-MRCP enjoys the merits of high special resolution and short acquisition time, and thus can be considered as the first choice in the patients have irregular breath patten. The conventional NT-MRCP should also be used when the images obtained by BH CS-MRCP show morphological consistency. Compared with BH CS-MRCP, BH-MRCP with parallel imaging yielded significantly better visualization of the segment 2 and 3 branch of the intrahepatic duct, and could be performed if the detail morphology information is necessary for diagnose.Acknowledgements
The authors thank the members of abdominal magnetic resonance team at Fujian Medical University Union Hospital.References
1. Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics 2009;29:1669–1688.
2. K. Liu, P. Xie, W. Peng, Z. Zhou, Magnetic resonance cholangiopancreatography: comparison of two- and three-dimensional sequences for the assessment of pancreatic cystic lesions, Oncol. Lett. 9 (2015) 1917–1921.
3. Chen Z, Sun B, Duan Q, et al. Three-Dimensional Breath-Hold MRCP Using SPACE Pulse Sequence at 3 T: Comparison With Conventional Navigator-Triggered Technique. AJR Am J Roentgenol. 2019 Dec;213(6):1247-1252.
4. Feng L, Benkert T, Block KT, Sodickson DK, Otazo R, Chandarana H. Compressed sensing for body MRI. J Magn Reson Imaging 2017;45(4):966–87.
Figures