1901
Value of MRCP in Santorinicele and Wirsungocele
Xinzhu Zhao1, Xing Wan1, Min Luo1, Mu Du1, Zhongxian Yang1, Qiuxia Xie1, Qian Zou1, Aiwen Guo1, Yingjie Mei2, and Yubao Liu1
1Medical Imaging Center, Shenzhen Hospital of Southern Medical University, Southern Medical University, Shenzhen, China, 2Philips Healthcare, Guangzhou, China
1Medical Imaging Center, Shenzhen Hospital of Southern Medical University, Southern Medical University, Shenzhen, China, 2Philips Healthcare, Guangzhou, China
Synopsis
The study investigated the potential association among pancreatitis, pancreas divisum (PD), and santorinicele or wirsungocele (two types of pancreatic ductal variations) based on three-dimensional magnetic resonance cholangiopancreatography (3D-MRCP). The clinical and imaging samples of 75 patients were collected and sorted into santorinicele and wirsungocele groups. Potential factors related to wirsungocele and santorinicele were investigated. MRCP showed good performance in visualizing ductal anomalies. Patients with santorinicele had higher risks of developing pancreatitis compared with those with wirsungocele. Additionally, santorinicele itself might be more closely associated with pancreatitis than with PD.
Introduction
Santorinicele and wirsungocele are rare anomalies characterized by the cystic dilatation of the terminal portion of the dorsal (santorini) or ventral (wirsung) pancreatic duct. Pancreas divisum (PD) is the lack of fusion between the dorsal and ventral pancreatic anlagen. Previous studies explored the association between pancreatitis and santorinicele/PD; however, the conclusions were contradictory. Also, a systematic evaluation on wirsungocele was lacking (1-3).The purpose of this study was to investigate the potential associating association among pancreatitis, pancreas divisum (PD), and santorinicele or wirsungocele (two types of pancreatic ductal variations) based on three-dimensional magnetic resonance cholangiopancreatography (3D-MRCP).Materials and Methods
This retrospective study was approved by the local ethics review and comprised 75 participants according to the flow chart. The magnetic resonance imaging examinations were performed on either 1.5T (Signa, General Electric, Japan) or 3.0T (Ingenia, Philips Healthcare, Best, Netherlands) unit. The MR protocols included three-dimensional magnetic resonance cholangiopancreatography (3D-MRCP). For the 1.5T scanner, the 3D-MRCP sequencing was performed with T2-weighted fast recovery fast spin-echo under breath-triggering conditions. For the 3T scanner, the 3D-MRCP sequencing was performed with T2-weighted turbo spin-echo sequences after breath holding. All images were obtained in oblique coronal planes, and maximum intensity projection (MIP) image was reconstructed. All participants were divided into two groups: (1) santorinicele (n = 57); and (2) wirsungocele (n = 18). The 3D-MRCP sequence was acquired. Images were evaluated for the presence of santorinicele, wirsungocele, and PD. The states of pancreatitis were assessed according to the clinical and imaging instructors (4,5). The diagnostic sensitivity of MRCP was calculated. ERCP/EUS served as the reference standard. The chi-square and correlation tests were used to evaluate two groups with PD and pancreatitis. Subsets (a: patients with santorinicele developed pancreatitis; b: patients with santorinicele and PD did not develop pancreatitis; c: patients with santorinicele and PD developed pancreatitis) within the santorinicele group were assessed using the least significant difference (LSD) t test. An estimate of the relative risk of acquiring pancreatitis was calculated.Results
A total of 57 patients were included in the santorinicele group (14 men, 43 women; age range, 11–82 years; average age, 53.96 years), and 18 patients were included in the wirsungocele group (5 men, 13 women; age range, 23–78 years; average age, 56.39 years). As shown in Table1, the sensitivity of MRCP combined with MIP in detecting santorinicele and wirsungocele showed no difference (70.2% and 77.8%). PD is more common in patients with santorinicele than in those with wirsungocele(78.9% and 11.1%, P < 0.05, r = 0.599). Pancreatitis accounted for 59.6% in the santorinicele group, which was higher than that in the wirsungocele group (59.6% and 11.1%, P < 0.05, r = 0.416), and for those with santorinicele, the relative risk of pancreatitis was 5.368 (95%CI: 1.428–20.176). Patients with santorinicele tended to be younger than patients with santorinicele and PD after developing pancreatitis.Discussion
Previous studies acknowledged the value of MRCP in depicting ductal systems (6). In this study, MRCP showed relatively good sensitivity, but was still inferior to ERCP. The accuracy of MRCP has improved a lot with increasingly advanced techniques. Thus, it was assumed that MRCP could be comparable with continuous technique advancement. Many patients with pancreatitis were found to be santorinicele and PD variants, and still a part of them only had santorinicele. The result of this study supported previous findings that santorinicele and PD both had a high correlation with pancreatitis. Besides, this study demonstrated that compared with PD, santorinicele was more likely to induce pancreatitis in the early stage. Unlike santorinicele, wirsungocele might not cause pancreatitis directly but might leave people in a susceptible state.Conclusions
MRCP displayed potential in diagnosing subtle duct-related abnormalities. Patients with santorinicele had higher risks of developing pancreatitis than those with wirsungocele. In addition, santorinicele itself was associated more closely with pancreatitis than with PD. Clinically, when patients have recurrent idiopathic pancreatitis, it is of great importance to check for santorinicele as a potential cause.Acknowledgements
No acknowledgement found.References
Manfredi R, Costamagna G, Brizi MG, Spina S, Maresca G, Vecchioli A, Mutignani M, Marano P. Pancreas divisum and "santorinicele": diagnosis with dynamic MR cholangiopancreatography with secretin stimulation. Radiology 2000;217:403-8. 2. Abu-Hamda EM, Baron TH. Cystic dilatation of the intraduodenal portion of the duct of Wirsung (Wirsungocele). Gastrointest Endosc 2004;59:745-7. 3. Gonoi W, Akai H, Hagiwara K, Akahane M, Hayashi N, Maeda E, Yoshikawa T, Kiryu S, Tada M, Uno K, Okura N, Koike K, Ohtomo K. Santorinicele without pancreas divisum pathophysiology: Initial clinical and radiographic investigations. BMC Gastroenterol 2013;13:62. 4. Shimosegawa T, Kataoka K, Kamisawa T, Miyakawa H, Ohara H, Ito T, Naruse S, Sata N, Suda K, Hirota M, Takeyama Y, Shiratori K, Hatori T, Otsuki M, Atomi Y, Sugano K, Tanaka M. The revised Japanese clinical dFigures
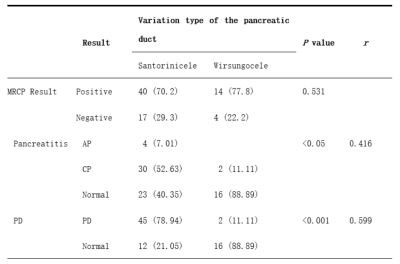
Table 1. The sensitivity of magnetic
resonance cholangiopancreatography and correlation analysis of santorinicele
and wirsungocele.Data
are numbers referring to the disease with the percentage in parentheses.
Chi-square tests were used to compare the difference in variation type in
different types of diseases. Cramer’s V coefficients were used to analyze
correlation.
MRCP, magnetic resonance cholangiopancreatography;
AP, Acute pancreatitis; CP, chronic pancreatitis; PD, pancreas divisum.
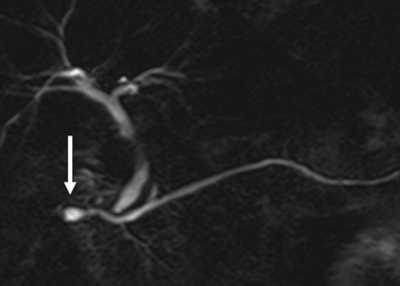
Figure 1. Santorinicele
visualized as a saccular dilatation of the distal dorsal duct just proximal
to the minor papilla (white arrow); ventral ductal invisible indicates a
complete pancreas divisum.

Figure 2. Wirsungocele
visualized as a saccular dilatation of the distal ventral duct just proximal to
the major papilla (white arrow).
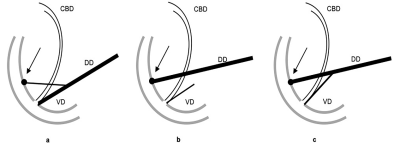
Figure 3. Santorinicele
with and without pancreas divisum.
Santorinicele
was defined as a focal saccular dilatation of the terminal end of the dorsal
pancreatic duct (arrows) and classified into two patterns according to the
presence or absence of pancreas divisum: (a) santorinicele without pancreas
divisum, (b) santorinicele with complete pancreas divisum; and (c)
santorinicele with incomplete pancreas divisum. CBD, Common bile duct; DD,
dorsal (pancreatic) duct; VD, ventral (pancreatic) duct.
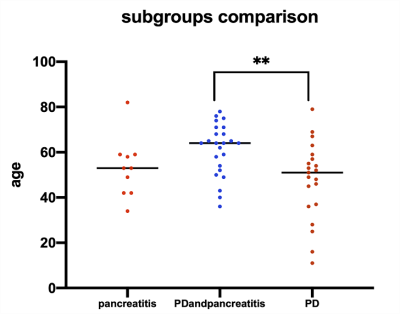
Figure 4. Comparison
of the average age between subgroups within the santorinicele group.
Subgroups
including (a) pancreatitis; (b) PD and pancreatitis; (c) PD.
**LSD
t test was used and P value <0.05.
PD, Pancreas divisum.