1899
A single breath-hold abdominal diffusion-weighted imaging with simultaneous multislice echo-planar imaging1Kanazawa University, Kanazawa, Japan, 2Philips Japan, Tokyo, Japan
Synopsis
Although respiratory-triggered (RT)-diffusion-weighted
imaging (DWI) has often been used to minimize respiratory motion in abdomen, unstable
respiration leads to prolonged scan time without resolving the problem of
respiratory motion. Therefore, we proposed a single breath-hold (BH)-DWI with
simultaneous multislice (SMS) echo-planar imaging to allow faster acquisition
and reliable quantification of apparent diffusion coefficient (ADC) in
abdominal DWI. The BH-DWI with SMS technique reduced the scan
time by more than fourfold and demonstrated comparable accuracy and
repeatability in ADC quantification with conventional RT-DWI. The proposed
method enables to acquire abdominal diffusion-weighted images in a single
breath-holding.
INTRODUCTION
Diffusion-weighted imaging (DWI) of the abdomen has been widely used for the detection and diagnosis of abdominal lesions.1 Moreover, the apparent diffusion coefficient (ADC) calculated from DWI with two or more b-values provides quantitative information on the diffusivity of water molecules in tissues. In free-breathing DWI, the respiratory motion of abdominal organs can reduce the image quality and could cause the misregistration between images with different b-values, resulting in the low accuracy of ADC measurement.2 Respiratory-triggered (RT)-DWI has often been used to minimize the effect of respiratory motion in abdomen3; however, the success of respiratory triggering depends on the consistency of the patient’s respiratory cycle (i.e., unstable respiration leads to prolonged scan time without resolving the problem of respiratory motion). Therefore, we proposed a single breath-hold (BH)-DWI with simultaneous multislice (SMS) echo-planar imaging (EPI) to allow faster acquisition and reliable ADC quantification in abdominal DWI.MATERIALS AND METHODS
On a 3.0-T magnetic resonance imaging (MRI) system, quantitative imaging biomarker alliance (QIBA) diffusion phantom consisting of 13 vials with various concentrations of polymer polyvinylpyrrolidone in aqueous solution was scanned with BH- and RT-DWI protocols. In BH-DWI, the SMS technique with an acceleration factor of 2 and reduced number of signals averaged (NSA) of 2 was used to keep the scan time within 23 s, which is practical for BH acquisition. In RT-DWI, an NSA of 4 was used, and the repetition time (TR) was set at 5000 ms, which simulated a normal respiration cycle and was different from the TR in BH-DWI (2500 ms). Other imaging parameters were kept constant between the protocols as follows: pulse sequence, single-shot diffusion EPI; echo time, 55 ms; slice thickness, 6 mm; number of slices, 30; field of view, 360 mm; imaging matrix, 128 × 128; sensitivity encoding factor, 2; half-scan factor, 0.7; and b-values, 0 and 800 s/mm2. Transverse images of the phantom were obtained with BH- and RT-DWI protocols, and the ADC maps were subsequently created. Then, we evaluated the signal-to-noise ratio (SNR), geometric distortion (GD), and ADC of each vial in the phantom according to the standards of the National Electrical Manufacturers Association.4 The SNR, distortion, and ADC were compared between both protocols using the Wilcoxon signed-rank test.On the same 3.0-T MRI system, nine healthy volunteers (all men) were scanned twice with BH- and RT-DWI to evaluate the repeatability of ADC measurement. Transverse abdominal images were obtained with the same protocols as the phantom study, except for the TR in RT-DWI: the TR changed depending on patient’s respiration cycle. Regions of interests (ROIs) were manually drawn in the liver, renal cortex, paraspinal muscle, spleen, and pancreas, and the ADC values were measured. Focusing on the ROI should be done carefully to avoid large vessels and subcutaneous fat. Then, the coefficient of variation (CV) of the ADC was calculated from the two scans to evaluate the repeatability. The ADC and CV were compared between both protocols using the Wilcoxon signed-rank test. A P value of < 0.05 was considered statistically significant.
RESULTS AND DISCUSSION
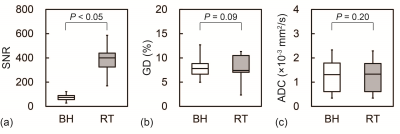
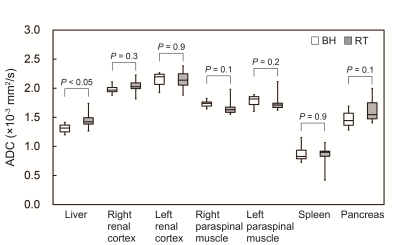
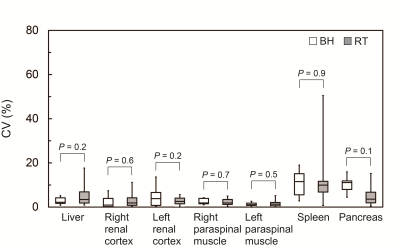
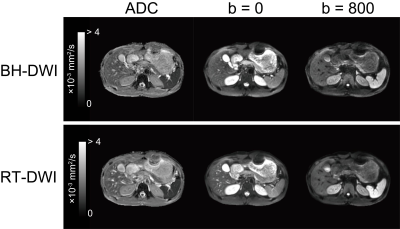
In the phantom study, compared with RT-DWI, BH-DWI reduced the scan time by 25%. Figure 1 shows the results of the SNR, GD, and ADC in the phantom. The SNR of BH-DWI was significantly lower than that of RT-DWI, with a mean SNR reduction of 76% ± 5% (P < 0.05). However, the GD and ADC did not significantly differ between both protocols. These results indicate that significant SNR penalty associated with substantial scan time reduction in BH-DWI did not affect the GD of images and the accuracy of ADC quantification. Although ADC is biased in insufficient SNR, leading to the underestimation of the ADC, the consistency in the ADC between both protocols supports the notion that SNR in BH-DWI was sufficiently high to ensure accurate ADC estimation.5In the volunteer study, the scan times were 23 s for BH-DWI and 165 s ± 28 s for RT-DWI, respectively. Figures 2 and 3 show the results of the ADC and CV in healthy volunteers. The ADC of the liver in BH-DWI was significantly lower than that in RT-DWI (P < 0.05). The mean difference in the ADC of the liver between BH- and RT-DWI was 9% ± 9%. A possible reason for the difference is the shorter TR (2500 ms) used in BH-DWI than in RT-DWI (i.e., 3000–5000 ms depending on the subject’s respiration cycle); it may be attributed to the decrease in the ADC of the blood in small hepatic vessels, which has a long T1 (1700 ms)6 and may have contaminated the liver ROI. By contrast, no significant differences were found in the ADCs of other regions between BH- and RT-DWI. Moreover, no significant differences were observed in the CV of the ADC between BH- and RT-DWI in all regions. These results suggest that the repeatability of ADC in BH-DWI is comparable with that in RT-DWI.
CONCLUSION
The BH-DWI with SMS technique reduced the scan time by more than fourfold and demonstrated comparable accuracy and repeatability in ADC quantification with conventional RT-DWI. The proposed method enables abdominal DWI in a single breath-holding.Acknowledgements
References
1. Thoeny HC, De Keyzer F. Extracranial applications of diffusion-weighted magnetic resonance imaging. Eur Radiol 2007;17:1385-1393.
2. Nasu K, Kuroki Y, Sekiguchi R, et al. The effect of simultaneous use of respiratory triggering in diffusion-weighted imaging of the liver. Magn Reson Med Sci 2006;5:129-136.
3. Kandpal H, Sharma R, Madhusudhan KS, et al. Respiratory-triggered versus breath-hold diffusion-weighted MRI of liver lesions: comparison of image quality and apparent diffusion coefficient values. AJR Am J Roentgenol 2009;192:915-922.
4. National Electrical Manufacturers Association (NEMA). NEMA Standards Publication MS 1-2008; 2008.
5. Walker-Samuel S, Orton M, McPhail LD, et al. Robust estimation of the apparent diffusion coefficient (ADC) in heterogeneous solid tumors. Magn Reson Med 2009;62:420-429.
6. Li W, Grgac K, Huang A, et al. Quantitative theory for the longitudinal relaxation time of blood water. Magn Reson Med 2016;76:270-281.
Figures