1860
Brain response to acupuncture treatment in dysmenorrhea: An arterial spin labeling study1Department of Biomedical Imaging and Radiological Science, China Medical University, Taichung, Taiwan, 2Graduate Institute of Acupuncture Science, China Medical University, Taichung, Taiwan
Synopsis
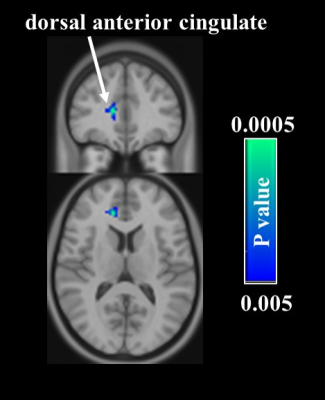
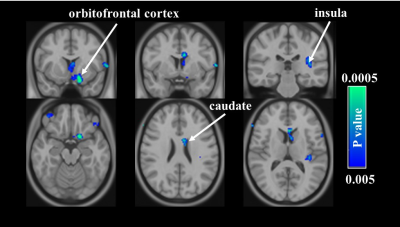
Studies on the brain responses to the pain-relieving treatments are relative limited, especially in dysmenorrhea. In this study, we investigated the brain response to acupuncture treatment in dysmenorrhea by using the arterial spin labeling technique. Results showed that after acupuncture treatment, significant decreases in cerebral blood flow were found in the pain-related regions, such as dorsal anterior cingulate cortex in the acupuncture group while orbitofrontal cortex, caudate, and insula in the sham acupuncture group. These findings suggest that acupuncture improves the descending pain modulation system by decreasing the neuronal activity in these brain regions.
Introduction
Dysmenorrhea is the occurrence of painful menstrual cramping of the uterus, and affects as many as 85% of women1. Standard treatments for dysmenorrhea including nonsteroidal anti-inflammatory drugs and hormonal contraceptive methods are used to exert the hypoalgesic action2. However, the side effects such as gastrointestinal complaint and mild neurological symptoms may deter some females from these medications3. Acupuncture has been considered as an alternative treatment for dysmenorrhea in the East Asia for the past 20 years. The beneficial effects of acupuncture include increasing participation in daily activities and reducing the amount of pain medication ingested4. Nevertheless, it has been shown that the treatment effect of acupuncture is primarily associated with the placebo effect, and the degrees of the efficacy depend on the subject’s perceptions and expectations. To understand the effect of acupuncture on analgesic actions in dysmenorrhea, we noninvasively explore the whole brain perfusion response to the acupuncture treatment by using the arterial spin labeling (ASL) technique. Findings from this work will shed more light on the mechanism underlying the role of acupuncture in pain relief.Methods
Study design: Twenty-three dysmenorrhea subjects participated in this study (age: 20-31 years old). All the subjects have a regular menstrual cycle of 27 to 35 days. Subjects were randomly divided into the acupuncture (N=11) and sham acupuncture groups (N=12), respectively. Subjects in the acupuncture group received the acupuncture treatment at the acupoints of bilateral Sanyinjiao (SP6) for eight weeks. The sham treatment consisted of the non-penetrating acupuncture at the same acupoints used in the acupuncture group. Subjects in both groups were scanned before and after the treatments, and the McGill pain questionnaire (MPQ) was also used to assess the psychological status before and after the treatment. Informed consent was obtained using IRB-approved protocol. MRI measurement: Magnetic resonance imaging was performed at a 3T scanner (GE, Signa, Excite HDxt, Wisconsin, USA). The MRI protocol consisted of a T1-weighted fast spoiled gradient echo (FSPGR) and a pseudo-continuous arterial spin labeling (pCASL) sequence. The scan parameters of the FSPGR sequence were as follows: TR/ TE/flip angle=8.02 ms/2.99ms/12°, TI = 450ms, spatial resolution = 1 × 1 × 1 mm3, and number of slices = 170. Scan parameters of the pCASL sequence were as follows: TR/ TE/ flip angle=4600 ms/9.8ms/12°, post labeling delay = 1.8 s, labeling duration = 1.5 s, and 30 pairs of label and control images. Data analysis: To quantify the perfusion-weighted maps of the pCASL sequence as CBF maps, a single-compartment model was used. All the CBF maps were normalized to the MNI space. A paired t-test was performed to examine the differences in voxelwise CBF and MPQ responses before and after treatment for both groups.Results and Discussion:
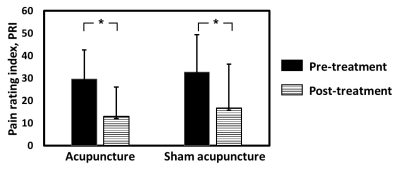
Assessment of psychological status: The results of MPQ of the total pain rating index (PRI) are displayed in Fig. 1. In the acupuncture group, the PRI before and after intervention were 29.5 ± 13 and 19.2 ± 13, respectively. In the sham group, the PRI before and after intervention were 32.6 ± 16.7 and 20.6 ± 19.4, respectively. The PRI was significantly decreased in both groups (both P < 0.05), suggesting the analgesic effect of both acupuncture and sham acupuncture on dysmenorrhea. CBF voxelwise analyses: We then analyzed regional CBF maps measured with ASL MRI to examine which brain regions manifested the acupuncture-associated alterations. In the acupuncture group, voxelwise analyses suggested that decreases in CBF were most significant in the right dorsal anterior cingulate cortex (dACC) after the treatment (Fig. 2). Response in dACC is commonly observed in studies of pain5. In the sham acupuncture group, it can be seen that after the treatment, the reductions in CBF were clearly demonstrated in other pain-related regions such as orbitofrontal cortex, caudate, and insula (Fig. 3). The development of dysmenorrhea could be ascribed to increased activity in these pain-related regions6. Therefore, the observed decrease in CBF is consistent with the possibility that acupuncture improves the descending pain modulation system by decreasing the neuronal activity in these brain regions.Conclusion
This exploratory study investigated the brain response to acupuncture treatment in dysmenorrhea using the noninvasive ASL technique. Although the mechanisms of acupuncture and sham acupuncture are dissimilar as manifested by the different brain responses, findings in this study provide some new information regarding the beneficial effects of acupuncture on dysmenorrhea and these effects may be explained by decreasing CBF to mediate the perception of nociceptive input.Acknowledgements
No acknowledgement found.References
1. Klein, J.R.; Litt, I.F. Epidemiology of adolescent dysmenorrhea. Pediatrics 1981, 68, 661-4.
2. Dawood, M.Y. Primary dysmenorrhea: advances in pathogenesis and management. Obstetrics and gynecology 2006, 108, 428-41.
3. Marjoribanks, J.; Proctor, M.; Farquhar, C.; Derks, R.S. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. The Cochrane database of systematic reviews 2010, CD001751.
4. Chao, M.T.; Wade, C.M.; Abercrombie, P.D.; Gomolak, D. An innovative acupuncture treatment for primary dysmenorrhea: a randomized, crossover pilot study. Alternative therapies in health and medicine 2014, 20, 49-56.
5. Lieberman, M.D.; Eisenberger, N.I. The dorsal anterior cingulate cortex is selective for pain: Results from large-scale reverse inference. Proceedings of the National Academy of Sciences of the United States of America 2015, 112, 15250-5.
6. Zhang, Y.N.; Huang, Y.R.; Liu, J.L.; Zhang, F.Q.; Zhang, B.Y.; Wu, J.C.; Ma, Y.; Xia, J.; Hao, Y.; Huo, J.W. Aberrant resting-state cerebral blood flow and its connectivity in primary dysmenorrhea on arterial spin labeling MRI. Magnetic resonance imaging 2020, 73, 84-90.
Figures