1859
Changes of brain perfusion under anesthesia in humans – an explorative Arterial Spin Labeling study
Thomas Lindner1,2, Hajrullah Ahmeti3, Dana Voß3, Monika Huhndorf2, Friederike Austein1,2, Michael Helle4, Olav Jansen2, Michael Synowitz3, and Stephan Ulmer2,5
1Department of Diagnostic and Interventional Neuroradiology, University Hospital Hamburg-Eppendorf, Hamburg, Germany, 2Department of Radiology and Neuroradiology, University Hospital Schleswig-Holstein, Kiel, Germany, 3Neurosurgery, University Hospital Schleswig-Holstein, Kiel, Germany, 4Tomographic Imaging Department, Philips Research Laboratories, Hamburg, Germany, 5Radiology, Kantonsspital Winterthur, Winterthur, Switzerland
1Department of Diagnostic and Interventional Neuroradiology, University Hospital Hamburg-Eppendorf, Hamburg, Germany, 2Department of Radiology and Neuroradiology, University Hospital Schleswig-Holstein, Kiel, Germany, 3Neurosurgery, University Hospital Schleswig-Holstein, Kiel, Germany, 4Tomographic Imaging Department, Philips Research Laboratories, Hamburg, Germany, 5Radiology, Kantonsspital Winterthur, Winterthur, Switzerland
Synopsis
Arterial Spin Labeling allows to intraoperatively monitor changes in perfusion induced by anesthesia.
Introduction
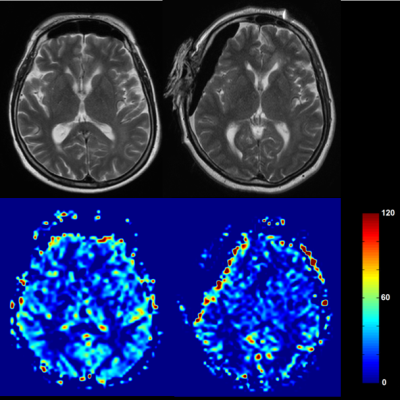
The use of intraoperative imaging devices may aid surgeons in decision making during surgery to improve safety, efficiency and clinical outcome. Magnetic Resonance Imaging (MRI) is unchallenged in its soft tissue contrast and recently, the use of Arterial Spin Labeling (ASL) perfusion imaging was shown as a valuable addition to routine scanning for the evaluation of residual tumors in glioblastoma surgery1. Due to the more invasive nature of other perfusion imaging methods using external contrast agents, it is nearly impossible to obtain data from patients before and under anesthesia. Thus, in this study, ASL was used to evaluated the influence of anesthesia.Materials and Methods
The patient collective consists of 15 patients (4 women, 11 men, mean age 51.4 years) suffering from Glioblastoma Multiforme (GBM) who underwent scanning prior to surgery on either a 3T or 1.5T Achieva scanner and intraoperatively on a 1.5T Intera scanner (all from Philips Healthcare, Best, The Netherlands). The study was approved by the local ethical committee. Scan parameters included: 1800ms labeling duration and post labeling delay, 2D multislice EPI scanning with 3.6x3.5x5mm³ resolution, TR/TE: 2616/13ms, 20 label/control pairs at 3T and 40 at 1.5T. All data was quantified in terms of ml/min/100g based on the formula presented in the ASL consensus paper2. Gray matter CBF was evaluated in the healthy hemisphere. The presented values represent the hemisphere average.Results and Discussion
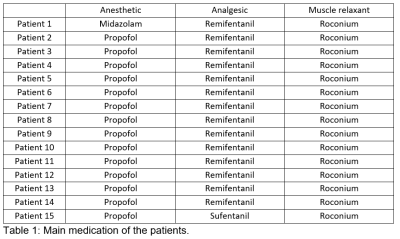
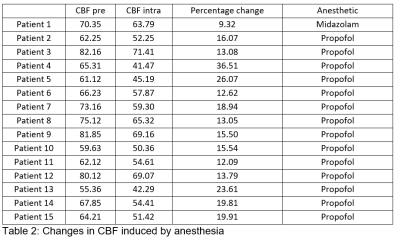
14 patients received propofol as anesthetic and one midazolam. The muscle relaxant and analgesic are shown in table 1. All patients had a reduced CBF, the patient with midazolam 9.32%, the others between 13.05% up to 36.51% (mean: 18.33% std. dev. 6.5%) indicating that anesthesia reduces CBF systemetically in the brain. Students’ t-test showed a p-value of <0.01 comparing pre- and intraoperative CBF values.Conclusion
While this is an exploratory study on the effects of anesthesia on brain perfusion, the question remains whether this effect of significant reduction of CBF has any pathological or physiological long-term effects on the patients or there are no residual effects after recovering from surgery.Acknowledgements
No acknowledgement found.References
[1] Lindner T, Ahmeti H, Juhasz J, et al. A comparison of arterial spin labeling and dynamic susceptibility perfusion imaging for resection control in glioblastoma surgery. Oncotarget. 2018;9(26):18570-18577. Published 2018 Apr 6. doi:10.18632/oncotarget.24970
[2] Alsop DC, Detre JA, Golay X, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med. 2015;73(1):102-116. doi:10.1002/mrm.25197