1855
An increased Normal Appearing White Matter perfusion: a possible radiological inflammatory marker in relapsing-remitting multiple sclerosis1DINOGMI, University of Genoa, Genoa, Italy, 2Department of Experimental Neurosciences, Ospedale Policlinico San Martino IRCCS, Genoa, Italy, 3Department of Human Neurosciences, Sapienza University of Rome, Rome, Italy, Rome, Italy, 4Department of Clinical Experimental Oncology, IRCCS Regina Elena National Cancer Institute, IFO, Rome, Italy, Rome, Italy, 5Fatebenefratelli Foundation, Afar Division, Fatebenefratelli Hospital, Isola Tiberina, Rome, Italy, Rome, Italy, 6Neurology Unit, San Giovanni-Addolorata Hospital, Rome, Italy, Rome, Italy, 7Department Of Neuroscience Mental Health And Sensory Organs (NEMOS), Sapienza University, Sant’Andrea Hospital, Rome, Italy, Rome, Italy, 8Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, USA/, New York, NY, United States
Synopsis
Hemodynamic changes by Dynamic Susceptibility Contrast enhanced perfusion (DSC) in Multiple Sclerosis (MS) have been poorly evaluated. The aim of the study was to compare relapsing and remitting (RR) MS patients by DSC. 45 RRMS patients, 22 with (REL) and 23 without (REM) relapse in the previous 2 months were included. A hyperperfusion of the Normal Appearing White Matter (NAWM) compared to FLAIR lesions was noted. The correlations between NAWM perfusion, disease duration and 1-year before Annualized Relapse Rate in REM patients seemed to suggest that an increased NAWM perfusion may be a radiological marker of higher inflammatory activity.
Background
Multiple sclerosis (MS) is an inflammatory-degenerative disease of the central nervous system. Two hypothesis for brain haemodinamic changes in MS have been suggested: (i) the tissue damage due to inflammation may lead to a decreased metabolic demand for blood flow and (ii) a primary perivascular and vascular inflammation may cause microcirculation abnormalities1. Furthermore, several recent studies showed coagulation involvement in MS and, in particular, a pro-inflammatory status in patients with active with respect to patient with no active MS2. Dynamic Susceptibility Contrast enhanced (DSC) perfusion is an advanced MRI technique based on the regional susceptibility-induced signal loss caused by paramagnetic contrast agents on T2-weighted images. Evaluation of brain hemodynamic changes by DSC in MS have been performed in a few studies, generally comparing MS patients and healthy subjects, providing various results3-5. The aims of the study were (i) to compare relapsing and remitting (RR) MS patients by (i) assessing Cerebral Blood Flow (CBF), Cerebral Blood Volume (CBV) and Mean Transit Time (MTT) with DSC perfusion and (ii) to evaluate of the relationships among demographic/clinical features and MRI findings.Methods
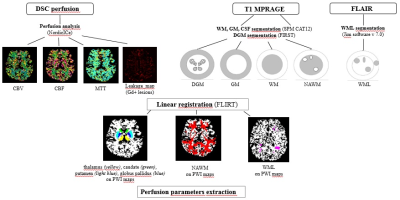
This is a multicenter, prospective, controlled study. We included RRMS patients in clinical relapse (REL) and those without relapse in the previous 2 months (REM). Demographic-clinical data were collected. All patients performed 3T MRI scan (GE, Waukesha, WI) including 3D-FLAIR, 3D-T1MPRAGE, DSC epiT2* and T1SE post gadolinium (GD) administration sequences. NordicIce software provided CBF, CBV and MTT maps. A leakage correction approach was performed to correct for GD extravasation in MS patients with evidence of GD lesions. MRI analysis pipeline is shown in Fig.1. Comparison between REL and REM groups were performed with Chi square and U-Mann Whitney tests were appropriate. Clinic-demographic features were correlated with radiological findings (Pearson’s test). ANOVA for repeated measures with Bonferroni correction was used to compare perfusion between FLAIR, T1 GD lesions and Normal Appearing White Matter (NAWM).Results
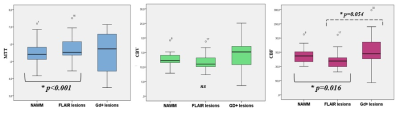
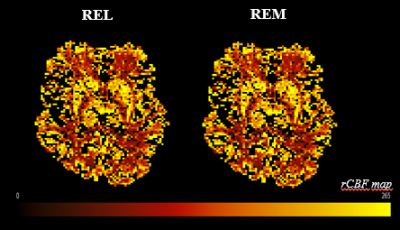
Up to date, 45 RRMS patients [(22 REL/23 REM); mean(SD) age 41.3(8.4); female 77.8 %; mean disease duration (DD) 12.8(7.1); median (IQR) EDSS 2 (1-5); mean Annualized Relapse Rate (ARR) last 1year and 2years before MRI date 0.7(1.2) and 0.4(0.7); mean cumulative number of relapses (CNR) 3.9(3.6). CNR, ARR 1y and 2y were significantly different between REL and REM (p<0.001 for all). By correcting for age and sex, FLAIR and T1 lesion load correlated with DD (p=0.001, r=0.8 and p<0.001, r=0.8, respectively), CNR (p<0.05, r= 0.6 for both FLAIR and T1) and z-MSFC (p<0.05, r=-0.7 for both FLAIR and T1). In REM group, correlations either between NAWM CBV and DD (p<0.05, r=-0.6) or between NAWM CBF and both DD (p=0.001, r=-0.7) and ARR-1y (p<0.05, r=0.4) were found. No significant correlations between FLAIR, T1 MPRAGE, GD lesion (volume and number) and NAWM perfusion parameters were noted. MTT was lower whereas CBF was higher in NAWM than in FLAIR lesions (p<0.05) (Fig.2). Applying leakage correction approach on patients with GD lesions (n=15) a trend indicating a higher perfusion of GD compared to FLAIR lesions was observed in CBF maps (p=0.054) (Fig.2). No significant differences in NAWM and deep gray matter perfusion between REL and REM were detected (Fig.3).Discussion
The evidence of microvascular involvement in MS has been reported by histological and MRI studies3, showing a “vasculitis” of the small veins with acute and chronic venous occlusion due to perivascular and intravascular fibrin deposition3. Few MRI perfusion studies in MS compared MS patients and healthy subjects, providing various results3-5. Dynamic haemodynamic changes and compensatory mechanisms that may occur in the brain vessels of MS patients due to inflammation and venous occlusion due to fibrin deposition may be an explanation of this issue3. In our study, including REL and REM MS patients, we demonstrated a relative hyperperfusion of NAWM compared to FLAIR lesions. A trend for a relative hyperperfusion of GD compared to FLAIR lesions was noted, probably not reaching a statistical significance due to the small number of GD lesions in our sample. In line with previous studies, no significant correlations between FLAIR, T1 MPRAGE, GD lesion (volume and number) and NAWM perfusion parameters were detected. This finding is not surprisingly, taking into account that occult and diffuse pathology in NAWM can occur independently of the presence of MRI visible lesions5. Finally, the correlations between NAWM perfusion, DD and ARR-1y in REM patients seemed to suggest that an increased NAWM perfusion may be a radiological marker of higher inflammatory activity.Conclusions
DSC perfusion technique may detect hemodinamic changes inside the brain of MS patients. Optimised processing techniques may reduce inter-raters variability in identifying the Region of Interest (ROIs) on perfusion maps with respect to ROIs visual tracing6. In our study, NAWM of RRMS patients seems to have higher perfusion than FLAIR lesions. A leakage correction approach seems to be appropriate to detect hemodinamic changes inside GD lesions, suggesting a higher perfusion of GD with respect to FLAIR lesions, possibly related to acute inflammation. Finally, also in patients with no relapses during the last two months, DSC perfusion seemed to be able to detect subtle changes in NAWM perfusion related to the inflammatory activity occurred in the previous year.Acknowledgements
No acknowledgement found.References
1. Adams RA, Passino M, Sachs BD, et al. Fibrin mechanisms and functions in nervous system pathology. Mol Interv 2004;4:163–176.
2. Plantone D, Inglese M, Salvetti M, et al. A Perspective of Coagulation Dysfunction in Multiple Sclerosis and in Experimental Allergic Encephalomyelitis. Front Neurol 2019 14;9:1175.
3. Law M, Saindane A, Ge Y, et al. Microvascular abnormality in relapsing-remitting multiple sclerosis: perfusion MR imaging findings in normal-appearing white matter. Radiology 2004; 231(3):645-52.
4. Ge Y, Law M, Johnson G, et al. Dynamic susceptibility contrast perfusion MR imaging of multiple sclerosis lesions: characterizing hemodynamic impairment and inflammatory activity AJNR Am J Neuroradiol 2005;26(6):1539-47.
5. Adhya S, Johnson G, Herbert J, et al. Pattern of hemodynamic impairment in multiple sclerosis: dynamic susceptibility contrast perfusion MR imaging at 3.0 T. Neuroimage 2006 Dec;33(4):1029-35. 6. Sowa P, Bjørnerud A, Nygaard GO, et al. Reduced perfusion in white matter lesions in multiple sclerosis Eur J Radiol. 2015; 84(12):2605-12.