1801
Liver parenchymal change after stereotactic radiotherapy for hepatocellular carcinoma using DWI and MRE1University of Yamanashi, Yamanashi, Japan, 2Kofu-Kyoritsu Hospital, Yamanashi, Japan
Synopsis
Stereotactic body radiotherapy (SBRT) is a treatment option for patients with hepatocellular carcinoma (HCC). It has been difficult to know radiation induced liver damage by SBRT using conventional imaging modalities. In this study, we evaluated the liver parenchymal changes after SBRT using two quantitative MR imaging; stiffness measurement with MR Elastography(MRE) and the apparent diffusion coefficient (ADC) values with DWI.Liver stiffness and ADC values were significantly elevated in both the liver parenchymal areas receiving large radiation dose (>30Gy) and small radiation dose(<15Gy). Liver stiffness and ADC values might be able to catch the substantial liver parenchymal changes after SBRT.
Introduction
Treatment options for patients with hepatocellular carcinoma (HCC) include liver transplantation, surgical resection, and percutaneous ablation therapy. Currently, stereotactic body radiotherapy (SBRT) is considered another treatment option for patients with HCC1. One of the major limitations of SBRT, however, is un-avoidable irradiation (at least 10 cGy) to non-target area of the liver parenchyma. Since it is not possible to quantitatively evaluate the liver damage by irradiation using conventional imaging modalities, this un-avoidable irradiation is a major concern for hepatologists. MR elastography (MRE) is a technique that evaluates organ stiffness, which is increased not only by fibrosis but also by inflammation2. ADC measurement is another quantitative method to evaluate liver parenchymal changes.This study aimed to evaluate the liver parenchymal changes after SBRT using MR-based quantitative method, liver stiffness and ADC values.Methods
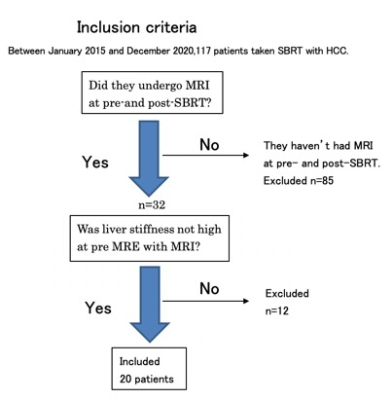
This retrospective study was approved by the relevant institutional review board, and informed consent was waived accordingly. We included 20 patients who received SBRT for HCC and underwent MRI with DWI and MRE at pre- and post-SBRT during the period between January 2015 and December 2020 (mean age, 76.9 years; range, 62–87; 17 men, 3 women). Patient and treatment characteristics are shown in Table1. MRI was performed using a 3-T MR system (Discovery 750; GE Medical Systems, Waukesha, WI, USA) with a 32-channel phased-array coil. SE-EPI based multi-slice MRE. We defined the liver area according to the radiation dose received by SBRT; area receiving high dose of radiation (>30Gy), low dose of radiation (<15Gy), and area between them. We obtained the region of interest (ROI) at high and low dose area to measure liver stiffness and ADC values. Wilcoxon signed-rank test (JMP ver.15) was used to compare the measured results between pre- and post-SBRT. The correlation was also evaluated between the rate of change in liver stiffness and ADC values.Result
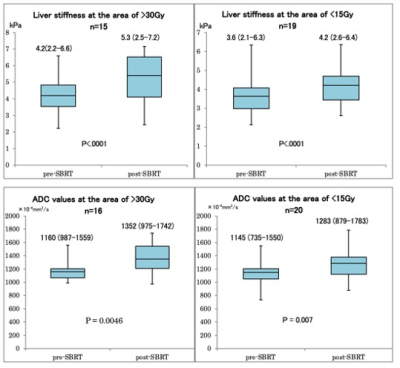
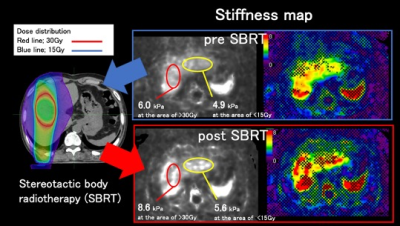
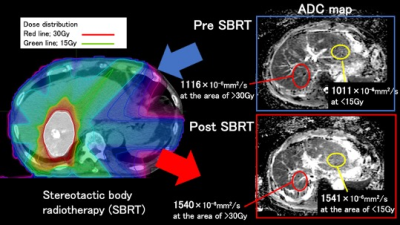
Liver stiffness and ADC values were significantly increased after SBRT in both areas (high dose area, p<.005; low dose area, p<.005). (Figure 2) There was no correlation between these two values.Discussion
In this study, we revealed the parenchymal changes after SBRT using MRE and DWI. In the results, liver stiffness was increased after SBRT by ~1.0kPa in the area of high dose and by ~0.5kPa in the area of low dose. In general, elevated stiffness indicate fibrosis or inflammation. In this study, the cause of elevation should be inflammation due to SBRT. ADC values of liver parenchyma were also increased after SBRT by ~200x10-6 mm2/s in the area of high dose and by ~140x10-6 mm2/s in the area of low dose. It may suggest that both liver stiffness and ADC values reflect parenchymal reaction or inflammation after SBRT. From this result, we may speculate that MRE and DWI can be used for evaluating the liver parenchymal effect by irradiation.Conclusion
Liver stiffness and ADC values of the liver parenchyma were significantly increased after SBRT.Acknowledgements
The authors gratefully acknowledge the assistance of Masahide Saito, Tomoko Akita, and Masaki Matsuda from University of Yamanashi Hospital.References
1) Takeda et al. Phase 2 Study of Stereotactic Body Radiotherapy and Optional Transarterial Chemoembolization for Solitary Hepatocellular Carcinoma Not Amenable to Resection and Radiofrequency Ablation. Cancer 2016; 2016;122:2041-9.
2) Arena U et al. Acute viral hepatitis increases liver stiffness values measured by transient elastography. Hepatology. 2008;47:380–384. doi: 10.1002/hep.22007.
Figures