1739
Feasibility of Single Breath-hold Isotropic Voxel 129Xe MRI in COVID-19 Survivors using a Key-Hole Method.
Tuneesh K. Ranota1, Hacene Serrai2, David G. McCormack3, Grace Parraga1,4,5, and Alexei Ouriadov1,2,6
1School of Biomedical Engineering, Faculty of Engineering, The University of Western Ontario, London, ON, Canada, 2Department of Physics and Astronomy, The University of Western Ontario, London, ON, Canada, 3Division of Respirology, Department of Medicine, The University of Western Ontario, London, ON, Canada, 4Robarts Research Institute, London, ON, Canada, 5Department of Medical Biophysics, The University of Western Ontario, London, ON, Canada, 6Lawson Health Research Institute, London, ON, Canada
1School of Biomedical Engineering, Faculty of Engineering, The University of Western Ontario, London, ON, Canada, 2Department of Physics and Astronomy, The University of Western Ontario, London, ON, Canada, 3Division of Respirology, Department of Medicine, The University of Western Ontario, London, ON, Canada, 4Robarts Research Institute, London, ON, Canada, 5Department of Medical Biophysics, The University of Western Ontario, London, ON, Canada, 6Lawson Health Research Institute, London, ON, Canada
Synopsis
Hyperpolarized 129Xe gas lung MRI is an efficient technique used to investigate and assess pulmonary diseases. To improve the performance of 129Xe MRI in lung imaging a method for high-resolution 3D static ventilation images using FGRE combined with the key-hole method in a single breath-hold, was proposed. This technique acquires high-resolution 129Xe 3D static ventilation isotropic-voxel images from the COVID-19 survivors in a single breath-hold. The SNR of the images allowed for the analysis of VDP. This study confirms the feasibility of using isotropic-voxel acquisition sequence in a single breath-hold MRI to study the effects of COVID-19 on the lungs.
Purpose
It has been shown that inhaled hyperpolarized gas MRI is a useful technique in the diagnosis and treatment plan for many pulmonary diseases. This includes chronic obstructive pulmonary disease (COPD),1 asthma2 and lung cancer.3 However, this technique still suffers from technical challenges,4 preventing it from finding a niche in clinical application. Data poor sensitivity restrains the development of several acquisition techniques,5 namely, isotropic voxel static-ventilation imaging, accelerated multiple b-value diffusion-weighting MRI,6 and accelerated simultaneous collection of 129Xe gas and 129Xe within lung tissue/blood. Nevertheless, by taking advantage of the recent improvement in xenon polarization, effort has been made to overcome the low image resolution problem, where isotropic-voxel high-resolution 3D 129Xe static-ventilation data were collected in a single 16sec breath-hold from the asthma subjects using FGRE sequence. It was demonstrated that the asthma isotropic-voxel high-resolution 3D 129Xe static-ventilation images showed sufficient SNR to generate ventilation-defect- percent7 (VDP) estimates.8 We hypothesize that the isotropic-voxel high-resolution 3D 129Xe static-ventilation images can be obtained by combining the traditional low-resolution data acquisition method1 with the keyhole approach.9 In this proof-of-concept study, we confirm the effectiveness of this idea, by obtaining both low/high-resolution 3D 129Xe data which were acquired from a small group of the COVID-19 survivors with sufficient SNR, enough to precisely calculate the VDP values.Methods
Three COVID-19 survivors with written informed consent provided to an ethics-board-approved study protocol, underwent spirometry and 1H/129Xe MRI scanning. 129Xe imaging was performed at 3.0T (MR750, GEHC, WI) using whole-body gradients (5G/cm maximum) and a commercial 129Xe quadrature-flex RF coil (MR Solutions, USA).8 Traditional resolution xenon static-ventilation images were acquired using a coronal plane 3D FGRE sequence (TE/TR/initial-flip-angle=1.5ms/5.1ms/1.3o, variable-flip-angle,10 Bandwidth=16kHz, reconstructed matrix size=128x128x16, and FOV=40x40x24cm3, voxel size=3x3x15mm3) as previously described.7 All images were acquired in breath-hold (<16 second) after inspiration of 1.0L of gas (129Xe/4He mixture, 30/70) from functional-residual-capacity. Pre- (baseline) and post-salbutamol data set acquired for each study subjects. Extra four traditional low-resolution static-ventilation images were acquired without a xenon breath-hold to obtain the noise data sets. Isotropic high-resolution-images with 3x3x3 voxel-size were obtained by sandwiching four noise data sets and one xenon signal data set (so the total number of slice was 80) and performing 3D Fast Fourier Transform starting with the z-direction following the key-hole technique steps.9 Hyperpolarized 129Xe gas (polarization=35%) was obtained from a turn-key, spin-exchange polarizer system (Polarean 9820 129Xe polarizer).11 1H MRI was performed as previously described.1 Image SNR was calculated for five central slices for each coronal view by selecting two regions of interest with similar size, one inside the lung with homogeneous signal and one outside the lung containing noise.12 VDP was generated using a semi-automated segmentation algorithm as previously described.7Results
Figures 1, 2 and 3 show the acquired (traditional) and reconstructed isotropic-voxel static-ventilation images in coronal view (Figures 1 and 2, baseline) and axial view (Figure 3, post-salbutamol) for one COVID-19 survivor. Table 1 summarizes demographic information, as well as imaging results including SNR and VDP for the isotropic-voxel and traditional resolution static-ventilation measurements of the COVID-19 survivors. The generated VDP estimates for the COVID-19 survivors were lower for the isotropic-voxel data compared the traditional resolution data. The pre- and post-salbutamol very similar for both cases except Survivors 1, where the post-salbutamol value was more than twice as large. The calculated mean SNR values of the five isotropic-voxel images of the COVID-19 survivors ranged between 26 and 29, and between 55 and 70 for isotropic-voxel and traditional data, respectively.Discussion and Conclusion
In this proof-of-concept study, we demonstrated that 3D isotropic-voxel 129Xe static-ventilation images can be acquired in a single 16 second breath-hold using the key-hole technique with sufficient SNR to analyze VDP. The small number of study subjects is the main limitation of this work, preventing us from deriving a reliable conclusion of the VDP estimate accuracy for the high-resolution case. However, the mean values of the high resolution VDP are comparable to the values reported in the literature obtained with asthma patients.8 Survivor 1 VDPs show a substantial difference between the pre and post cases. One possible explanation to this difference is the unfinished gas-inhalation during the post-salbutamol 129Xe MRI scan. Isotropic-voxel coronal SNR-values were consistent with values reported in the literature.7 The SNR-estimates for the high resolution isotropic-voxel images was approximately half of the traditional non-isotropic images, but with voxel-size five times smaller. A rigid and more homogenous coil13 combined with a phased-receive-array14 could substantially improve isotropic-voxel image quality and potentially replace the isotopically-enriched 129Xe with the natural-abundant xenon,15 and consequently, reduce the cost of 129Xe MRI for patients. It is known that presently, 129Xe lung MRI is translating towards a clinical tool, and has recently been approved and used as such in the UK.16 The North-American xenon consortium17 expects 129Xe MRI to be FDA (Food and Drug Administration) approved any moment from now, and this opens the door for better diagnoses, treatment planning and treatment assessment of patients with chronic lung, cardiac and neurodegenerative diseases. This study establishes the usefulness of 129Xe isotropic-voxel static-ventilation imaging with a 3D FGRE sequence within a single breath-hold scan, confirming previous studies conducted on other patients suffering from lung diseases.Acknowledgements
The authors would like to thank the research and financial supports received from Western Research Catalyst Grant and The COVID-19 Rapid Research Fund in Ontario.References
- Kirby, M., Pike, D., Coxson, H. O., McCormack, D. G. & Parraga, G. Hyperpolarized (3)He ventilation defects used to predict pulmonary exacerbations in mild to moderate chronic obstructive pulmonary disease. Radiology 273, 887-896, (2014).
- Svenningsen, S. et al. Sputum Eosinophilia and MRI Ventilation Heterogeneity in Severe Asthma. Am J Respir Crit Care Med, (2018).
- Hoover, D. A. et al. Functional lung avoidance for individualized radiotherapy (FLAIR): study protocol for a randomized, double-blind clinical trial. BMC Cancer 14, 934, (2014).
- Albert, M. S. et al. Biological magnetic resonance imaging using laser-polarized 129Xe. Nature 370, 199-201, (1994).
- Rao, M. R., Stewart, N. J., Griffiths, P. D., Norquay, G. & Wild, J. M. Imaging Human Brain Perfusion with Inhaled Hyperpolarized 129Xe MR Imaging. Radiology 286, 659-665, (2018).
- Westcott, A., Guo, F., Parraga, G. & Ouriadov, A. Rapid single-breath hyperpolarized noble gas MRI-based biomarkers of airspace enlargement. J Magn Reson Imaging 49, 1713-1722, (2019).
- Svenningsen, S. et al. Hyperpolarized (3) He and (129) Xe MRI: differences in asthma before bronchodilation. J Magn Reson Imaging 38, 1521-1530, (2013).
- Barker, A. L. et al. Feasibility of Single Breath-hold Isotropic Voxel 129Xe MRI in Patients [abstract]. ISMRM 19th Annual Meeting, Paris, France, 4142, (2019).
- Niedbalski, P. J. et al. Mapping and correcting hyperpolarized magnetization decay with radial keyhole imaging. Magn Reson Med 82, 367-376, (2019).
- Ouriadov, A. V., Lam, W. W. & Santyr, G. E. Rapid 3-D mapping of hyperpolarized 3He spin-lattice relaxation times using variable flip angle gradient echo imaging with application to alveolar oxygen partial pressure measurement in rat lungs. MAGMA 22, 309-318, (2009).
- Kaushik, S. S. et al. Diffusion-weighted hyperpolarized 129Xe MRI in healthy volunteers and subjects with chronic obstructive pulmonary disease. Magn Reson Med 65, 1154-1165, (2011).
- Dominguez-Viqueira, W., Ouriadov, A., O'Halloran, R., Fain, S. B. & Santyr, G. E. Signal-to-noise ratio for hyperpolarized (3)He MR imaging of human lungs: a 1.5 T and 3 T comparison. Magn Reson Med 66, 1400-1404, (2011).
- Farag A, Wang J, Ouriadov A, Parraga G & G., S. Unshielded and asymmetric RF transmit coil for hyperpolarized 129Xe human lung imaging at 3.0 T. In Proceedings of the 20th Annual Meeting of ISMRM, Melbourne, Australia, 1233, (2012).
- Chang, Y. V., Quirk, J. D. & Yablonskiy, D. A. In vivo lung morphometry with accelerated hyperpolarized (3) He diffusion MRI: a preliminary study. Magn Reson Med 73, 1609-1614, (2015).
- Stewart, N. J., Norquay, G., Griffiths, P. D. & Wild, J. M. Feasibility of human lung ventilation imaging using highly polarized naturally abundant xenon and optimized three-dimensional steady-state free precession. Magn Reson Med 74, 346-352, (2015).
- Wild, J. M. et al. P283 Hyperpolarised Gas MRI – a pathway to Clinical Diagnostic Imaging. Thorax 70, A220.223-A221, (2015).
- 129Xe MRI Clinical Trials Consortium. https://cpir.cchmc.org/XeMRICTC.
Figures
Table
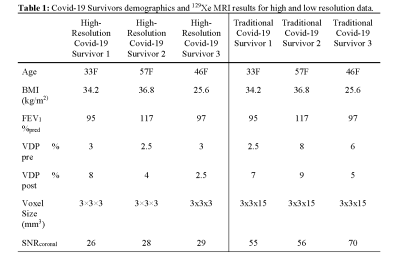
1: Covid-19 Survivors demographics and
129Xe MRI results for high and low resolution data. BMI=body
mass index, FEV1=forced expiratory volume in 1 second,
VDP=ventilation defect percent, SNR=signal to noise ratio, calculated for baseline
(pre-salbutamol) data only.
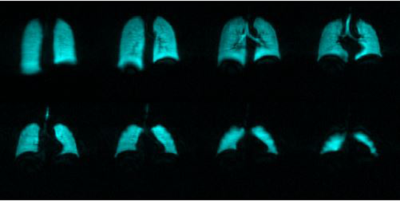
Figure
1: Coronal view of the traditional 129Xe
MRI static-ventilation slices from anterior to posterior for COVID-19 Survivor
1 (baseline).

Figure
2: Coronal view of the high resolution
isotropic 129Xe MRI static-ventilation slices from anterior to
posterior for COVID-19 Survivor 1 (baseline).
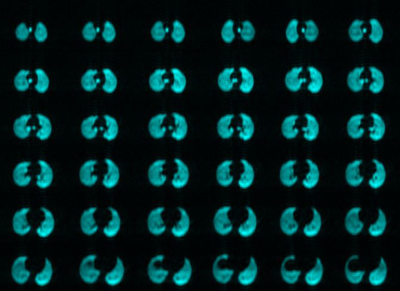
Figure 3: Axial view of the high resolution isotropic 129Xe
MRI static-ventilation slices from superior to inferior for COVID-19 Survivor 1
(post-salbutamol).