1648
Can 3D pseudo-continuous territorial arterial spin labeling effectively diagnose patients with recanalization of unilateral MCA stenosis?
Xinyu Wang1, Weiqiang Dou2, Xinyi Wang1, Kunjian Chen1, Huimin Mao1, and Yu Guo1
1Radiology department, The First Affiliated Hospital of Shandong First Medical University, Jinan, China, 2MR Research China, GE Healthcare, Beijing, China
1Radiology department, The First Affiliated Hospital of Shandong First Medical University, Jinan, China, 2MR Research China, GE Healthcare, Beijing, China
Synopsis
In this study, the main purpose was to explore the feasibility of 3D pseudo-continuous territory arterial spin labeling (tASL) in evaluating unilateral middle cerebral artery (MCA) recanalization. We included 47 patients with unilateral MCA stenosis diagnosed by DSA and performed tASL examination. Increased relative cerebral blood flow (rCBF) values were found in the blood supply area of MCA postoperatively than pre-operatively. Good prognosis was also revealed to closely associate with Alberta Stroke Program Early CT Score (ASPECTS) scores based on tASL perfusion images. Therefore, tASL can be used as one valuable method to diagnose the effect of vascular recanalization.
Synopsis
In this study, the main purpose was to explore the feasibility of 3D pseudo-continuous territory arterial spin labeling (tASL) in evaluating unilateral middle cerebral artery (MCA) recanalization. We included 47 patients with unilateral MCA stenosis diagnosed by DSA and performed tASL examination. Increased relative cerebral blood flow (rCBF) values were found in the blood supply area of MCA postoperatively than pre-operatively. Good prognosis was also revealed to closely associate with Alberta Stroke Program Early CT Score (ASPECTS) scores based on tASL perfusion images. Therefore, tASL can be used as one valuable method to diagnose the effect of vascular recanalization.Materials and Methods
Subjects47 patients (29 males vs 18 females; age: 54.3±12.0 years old) with unilateral MCA stenosis were included in this study. At admission, all patients were scored using the National-Institutes-of-Health-Stroke-Scale (NIHSS) and the modified Rankin-Scale (mRS) to assess the damage to central nervous system. At discharge, mRS<2 was defined as a good prognosis. All patients have undergone balloon dilation or stent implantation, and received MRI examinations before and after operation。
MRI experiment
All MRI experiments were performed on a 3.0T MRI scanner (GE Discovery 75, USA) equipped with a 32-channel head coil.
The scan parameters for tASL were: FOV=220m×220mm,slice thickness=4mm,TR/TE=4548/14.50ms, post-labeling-delay time=1525ms; for 3D-ASL were:TR/TE=4632/10.54ms, matrix=128 X 128, slice thickness=4mm, FOV =240mm×240mm, post-labeling delay time=1525ms. Total scan time was 9mins 23s.
The vascular markers selected in tASL measurement were a section of bilateral internal carotid arteries (ICAs) running perpendicular to the axial intracranial surface.
Image Analysis
All perfusion data were transferred to GE Advantage Workstation 4.6. A vendor-provided ASL post-processing software developed under FUNCTOOL platform was applied to analyze 3D-ASL and tASL images. The corresponding whole brain and vessel-specific cerebral blood flow (CBF) mapping were obtained.
Three symmetrical ROI regions were delineated on the maximum level of the bilateral MCA blood supply area of the CBF maps , with a range of (150±10) mm.The CBF values of ROI were measured and the mean values were calculated. According to the Alberta-Stroke-Program-Early-CT Score (ASPECTS) system evaluation, the perfusion area of MCA was divided into 10 perfusion areas per hemisphere, of which each area was counted for 1 point. When the perfusion was reduced, the number of corresponding areas were subtracted to obtain the score. The pseudo-color map of cerebral perfusion was visually analyzed to compare the cerebral tissue perfusion on both sides and diagnose the abnormal perfusion areas. For unevenly perfused lesions, the relative rCBF value was calculated based on the following equation: (rCBF=ischemic area CBF/contralateral mirror image CBF). The resultant rCBF ratio was considered normal, low and high perfusion at the value of 0.8-1.20, < 0.80, and > 1.20, respectively.
Statistical Analysis
All statistical analyses were performed using SAS software (SAS Institute Inc, NC). Paired t-test was separately used to compare rCBF difference of affected or contralateral side of MCA blood supply area before and after operation. Receiver-operating-characteristic curve (ROC) analysis and area-under-the-curve (AUC) were used to evaluate the diagnostic efficacy of 3D-ASL and tASL. Multivariate logistic regression analysis was performed on multiple factors including age, sex, hypertension, diabetes, smoking, drinking, previous stroke, NIHSS and ASPECTS score. Significant threshold was set as p <0.05.
Results
After recanalization, the rCBF values of the affected and normal side were significantly higher than the respective ones before operation (both P<0.05; Table1). A typical case is shown in Figure 1.Using ROC analysis, tASL imaging based on ASPECTS score has shown a good prognostic prediction (AUC=0.829; 95%CI: 0.651-1.000, P<0.05), while a lower prognostic value was observed with ASL imaging (AUC=0.760; 95%CI: 0.574-0.946, P <0.05, Fig.2). The difference analysis of each variable showed that the NIHSS score before recanalization and the scores based on ASPECTS score of ASL and tASL after recanalization were statistically different (P<0.05; Table.2). In multivariate analysis, ASPECTS scores based on ASL and tASL before and after surgery were considered as independent predictors of surgery prognosis (P<0.05,Table.3).Discussion and conclusions
In this study, we explored the feasibility of tASL in evaluating the perfusion changes after recanalization in patients with unilateral MCA stenosis or occlusion. Increased CBFs were shown in both sides after recanalization, indicating an improved cerebral ischemia condition. Additionally, we further divided the MCA perfusion area according to the ASPECTS score. Using ROC curve, ICA-specific tASL shows more robust diagnostic performance than whole brain ASL, because tASL perfusion is not affected by collateral circulation and compensation. In multivariate analysis, ASPECTS score based on perfusion images is high, confirmed as a predictor of good prognosis.Overall, with these findings, tASL can be demonstrated an effective tool for evaluating MCA recanalization.
Acknowledgements
No acknowledgement found.References
[1] Wang W, Jiang B, Sun H, et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480687 Adults [J]. Circulation, 2017, 135(8): 759-71.
[2] Song J, Ma Z, Meng H, et al. Distal hyperintense vessels alleviate insula infarction in proximal middle cerebral artery occlusion [J]. Int J Neurosci, 2016, 126(11): 1030-5.
[3] Hartkamp N S, Helle M, Chappell M A, et al. Validation of planning-free vessel-encoded pseudo-continuous arterial spin labeling MR imaging as territorial-ASL strategy by comparison to super-selective p-CASL MRI [J]. Magn Reson Med, 2014, 71(6): 2059-70.
[4] Hartkamp NS, Petersen ET, De Vis JB,et al. Mapping of cerebral perfusion territories using territorial arterial spin labeling: techniques and clinical application[J]. NMR Biomed. 2013,26(8):901-12.
Figures
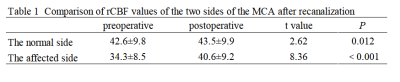
Table 1.Comparison of rCBF values of the two sides of the MCA after recanalization
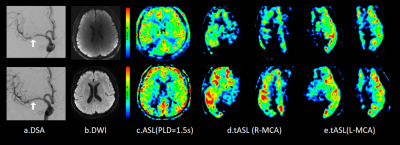
Figure 1. A patient with R-MCA undergoing stenting before (top row) and after (bottom row) surgery. A 65-year-old male with a severe R-MCA stenosis. a. DSA:after stenting, the stenosis of the R-MCA was significantly alleviated, the blood flow was recanalization.b. Preoperative ASL :low perfusion area was visible in M6, postoperative low perfusion basically returned to normal level. c.d. Preoperative tASL : the perfusion in M3, M5 and M6 areas was lower than the contralateral side, and the postoperative hypoperfusion area basically returned to normal level.
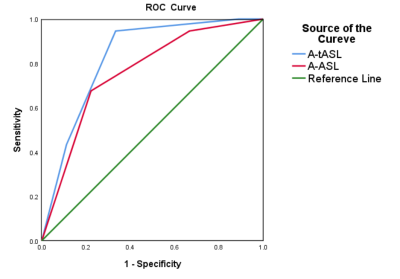
Fig 2 The ROC curve shows the sensitivity and specificity values for predicting good clinical outcomes with the ASPECTS score of ASL and tASL at various levels of cut-off scores. Predictive value of good prognosis based on the ASPECTS score in postoperative tASL technology(AUC=0.829;95%CI:0.651-1.000 P<0.05) higher than ASL (AUC=0.760;95%CI:0.574-0.946 P<0.05).
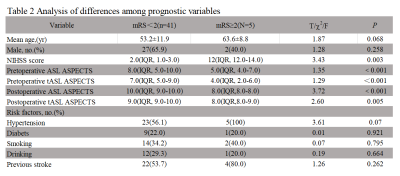
Table 2 Analysis of differences among prognostic variables
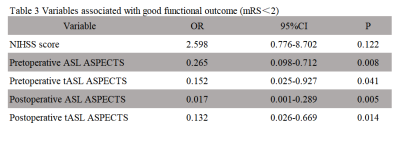
Table 3 Variables associated with good functional outcome (mRS<2)