1636
Morphological and hemodynamic alterations of major brain feeding arteries across the lifespan1Radiology, NYU Langone Health, New York, NY, United States, 2Vilcek Institute of Graduate Biomedical Science, New York University School of Medicine, New York, NY, United States, 3Radiology, Johns Hopkins University School of Medicine, Baltimore, MD, United States
Synopsis
Vascular dysfunction is frequently found in neurodegenerative and cerebrovascular diseases and closely related to age. Bilateral internal carotid arteries (ICAs) and vertebral arteries (VAs) are the key feeding vessels of the brain, which may provide important indices of intracranial health status. We aimed to evaluate age-related morphological and hemodynamic changes of the vessels using TOF MRA and phase contrast MRI. More tortuous appearance as well as reduced hemodynamics were observed with aging; Blood velocity was found to be associated with the morphology after adjusting age and gender, indicating that high blood velocity and wall shear stress could induce arterial tortuosity.
INTRODUCTION
Vascular dysfunction is a key characteristic of neurodegenerative and cerebrovascular diseases and has been found to be related closely to chronological age [1]. Arterial stiffening and deformation occur with aging caused by elasticity degradation and vascular wall remodeling as well as the changes of extracellular matrix and endothelium. It has been reported that vascular tortuosity could reduce blood flow and increase fluid shear stress, resulting in platelet activation and thrombosis [2]. Conversely, the vascular wall is sensitive to the hemodynamic forces imposed, and increased blood flow could lead to arterial tortuosity associated with elastin degradation and proinflammatory signaling activation [3, 4]. However, the explicit association between morphological variations and age remains obscure. Bilateral internal carotid arteries (ICAs) and vertebral arteries (VAs) are the key feeding vessels of the brain, and monitoring of their morphological and hemodynamic changes with clinical MRI may provide important indices of intracranial health status. This study aims to evaluate age-related morphological and hemodynamic changes of ICAs and VAs using TOF MRA and phase-contrast (PC) MRI.METHODS
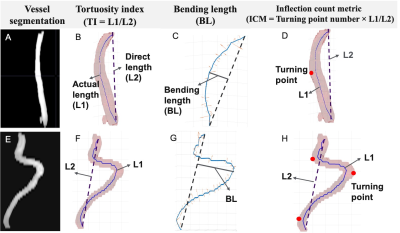
We studied 249 subjects, including 159 young subjects (age < 65, 41.2±13.28, 105 male/54 female) and 90 old subjects (age >= 65, 74.49±6.62, 56 male/34 female). Vessel morphology changes were evaluated on 3D TOF MRI (TR/TE = 23/3.45ms, FOV = 160×70×160mm3, voxel size = 1.0×1.0×15mm3, number of slices = 47, duration = 1 min 26 s). To quantitatively analyze the tortuosity changes, we first performed the vessel segmentation of ICAs, and VAs on TOF images and applied the fast marching algorithm to get the vascular skeleton [5, 6]. As described in Figure 1, tortuosity index (TI), bending length (BL), and inflection count metric (ICM) were proposed as morphological measurements for each vessel. The hemodynamic assessment was performed using 2D PC-MRI targeting for four feeding arteries at the level below cervical vertebrate C2 and above common carotid artery bifurcations with the following parameters (voxel size = 0.45×0.45×5 mm3, FOV = 230×230×5mm3, TR/TE = 20/7ms, VENC = 80 cm/s, duration = 30s). The velocity map image was computed from the phase difference between two scans with opposite signs of bipolar gradients, reflecting the signal from flowing spins. Blood flux, mean, and maximum blood velocity were then calculated. We applied t-test to compare morphological and hemodynamic features between young and old subjects. We also performed Pearson correlations between 1) age and morphological variables; 2) age and hemodynamic variables; 3) morphological and hemodynamic variables.RESULTS
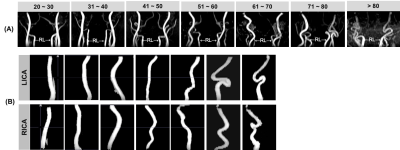
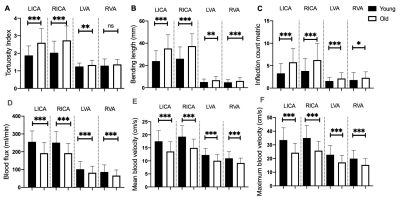
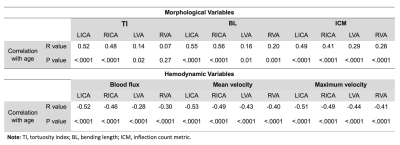
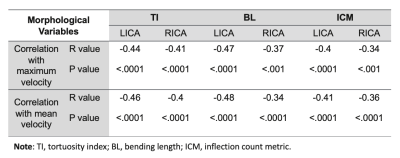
As shown in Figure 2, the increased vessel tortuosity is widely observed in the older subject groups. Compared to the younger subjects (<65 years old), older subjects had significantly higher TI, BL, and ICM values for bilateral ICA (p<.001), indicating the elderly have more twists and turns in their ICA course; however, the morphological indices measured for VAs were not as dramatic as ICAs (Figure 3). In addition, old subjects demonstrated significantly reduced hemodynamic measurements for all four vessels (p<.001) compared to young subjects (Figure 3). Consequently, total cerebral blood flow (CBF), as well as CBF normalized by the intracranial volume, were lower in old subjects (p<.001). The correlation results between morphological or hemodynamic measurements and age, including r values and p values were summarized in Table 1. Both morphological and hemodynamic measurements showed significant correlations with age. Correlations between morphological variables and hemodynamic variables were also calculated and reported in Table 2. LICA and RICA demonstrated significant negative correlations between maximum/mean velocity measured with PC-MRI and TI, BL, ICM morphological indices measured on TOF-MRI. After adjusting age and gender as covariates, blood flux had no association with all morphological parameters for all four extracranial vessels. For the vertebral artery system, only ICM was observed to be negatively correlated with maximum blood velocity (r = -0.21, P <.001) and mean blood velocity (r = -0.21, P <.001) within the LVA.DISCUSSION
To reveal the vessel alterations across the lifespan, we applied the MRI modality to decent cohort size. Older subjects demonstrated higher values of tortuosity indices and lower values of hemodynamic measurements for all vessels, indicating a higher degree of morphological changes and sluggish blood flow. The age-related vascular changes of the neck arteries are in accordance with previous reports on the middle cerebral artery tortuosity and diminished cerebral blood supply [7, 8]. The consequent hypoperfusion may be associated with age-related cognitive decline and neurodegenerative changes. We also observed the association between blood velocity and the morphological parameters, which indicates that high blood velocity and high wall shear stress could be protective factors for tortuosity alteration. There were many carotid artery ultrasound studies, of which the measurement variability is highly dependent on the angle of insonation and the anatomic location. The advantage of MRI over ultrasound is its smaller measurement variability [9]. The clinically accessible routine TOF and PC-MRI sequences applied in this study and their fast acquisition (< 5 minutes) make it potential to become a practical tool for clinical evaluation of neck vessel morphology and hemodynamics regarding intracranial health. By developing automated vessel segmentation method proposed in this study, more objective and quantitative analysis of individual vessel could be obtained, potentially providing decision-support tools in the clinical settingsAcknowledgements
This study was funded by the National Institute of Health grants (RF1 NS11041, R56 AG060822, R01 NS108491, R13 AG067684). This study is also supported by the Alzheimer’s Association (AARG-17-533484).References
1. El Assar M, Angulo J, Vallejo S, et al. Mechanisms involved in the aging-induced vascular dysfunction. Front Physiol. 2012;3: 132.
2. Chesnutt JK, Han HC. Tortuosity triggers platelet activation and thrombus formation in microvessels. J Biomech Eng. 2011;133(12): 121004-121004-11.
3. Langille BL. Arterial remodeling: relation to hemodynamics. Can J Physiol Pharmacol. 1996;74(7): 834-841.
4. Frösen J, Cebral J, Robertson AM, et al. Flow-induced, inflammation-mediated arterial wall remodeling in the formation and progression of intracranial aneurysms. Neurosurg Focus. 2019;47(1): E21.
5. Liu P, Lu H, Filbey FM, et al. Automatic and reproducible positioning of phase-contrast MRI for the quantification of global cerebral blood flow. PloS one. 2014;9(5), e95721.
6. Sethian JA. A fast marching level set method for monotonically advancing fronts. Proc Natl Acad Sci U S A. 1996;93(4): 1591-1595.
7. de La Torre JC. Cardiovascular risk factors promote brain hypoperfusion leading to cognitive decline and dementia. Cardiovasc Psychiatry and Neurol. 2012.
8. Virmani R, Avolio AP, Mergner WJ, et al. Effect of aging on aortic morphology in populations with high and low prevalence of hypertension and atherosclerosis. Comparison between occidental and Chinese communities. Am J Pathol. 1991;139: 1119-1129.
9. Duivenvoorden R, De Groot E, Elsen BM, et al. In vivo quantification of carotid artery wall dimensions: 3.0-Tesla MRI versus B-mode ultrasound imaging. Circ Cardiovasc Imaging. 2009; 2(3), 235-242.
Figures