1633
Developmental trajectories of cerebral blood flow and neurodevelopmental score in preterm children from 28 days to 13 years1First Affiliated Hospital of Xi 'an Jiaotong University, Xi'an, Shaanxi, China, 2MR Research China, GE Healthcare, Beijing, China
Synopsis
Preterm children often accompany undesirable neurodevelopmental outcomes. Adequate cerebral blood flow (CBF) is essential to brain development and function. However, little is known about relationship among preterm birth, CBF and neurodevelopmental outcome. This study aims to investigate the effect of preterm birth on CBF and explore the relationship between CBF and neurodevelopmental score. Our results suggest that the effects of preterm birth on intellectual development are long lasting and extend even into late childhood. After controlling for age, CBF shows positive correlations with mental and psychomotor development indexes in left frontal and occipital lobes in preterm children.
Main Findings
Preterm children showed lower cerebral blood flow than term in the frontal lobe, even at late childhood. After controlling for age, CBF showed positive correlations with mental and psychomotor development indexes in left frontal and occipital lobes in preterm children.Introduction
Preterm birth may cause cognitive development disorders, affecting children's academic and social adaptability. A sufficient and stable blood flow to the brain is essential for brain function and development. Previous studies have demonstrated that CBF in preterm infants is lower than that in full-term infants1. However, little is known about the relationship among preterm birth, CBF and neurodevelopmental outcome. Therefore, this study aims to investigate the effect of preterm birth on CBF and further explore the relationship between CBF and neurodevelopmental score.Methods
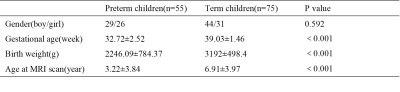
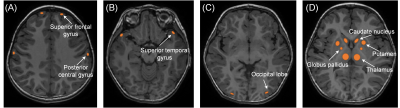
This study was approved by the local Internal Review Board and written informed consent was obtained from all children’s parents before MRI scanning. Patients 129 subjects (55 preterm children and 75 matched term children) were included, and the age ranged from 28 days to 13 years. (Table 1) Term children were born at full term without abnormalities in brain MR images. Meanwhile, we applied Bayley Scales of Infant development II (BSID II) to measure the mental development index (MDI) and psychomotor development index (PDI) of 16 preterm children aged 60 days to 4 years. MR Protocols Images were acquired on a 3.0T scanner (Signa HDxt, GE Healthcare, Milwaukee, WI, USA) with 8-channel head coil. The protocols included: (1) transverse 3D T1-weighted sequence (TR/TE,10ms/4.6ms; matrix, 256×256; section-thickness, 1mm; FOV, 240mm); (2) 2D T2-weighted sequence (TR/TE, 4200ms/120ms; matrix, 256×256; section-thickness,4mm; FOV, 240mm); (3)3D PCASL sequence (TR/TE, 4642ms/10.3ms; matrix, 288×192; section-thickness,4mm; FOV, 200mm;PLD,1525ms).Data and statistical analysis The CBF map was computed in mL/100g/minute from the ASL sequence with vendor provided software (Functool version 9.4, GE Healthcare). Manual regions of interest (ROIs) were placed on the CBF map by using the aligned anatomical image as guidance. Our ROIs involved cortex (bilateral frontal parietal temporal occipital lobe) and basal ganglia (bilateral thalamus, globus pallidus, putamen, caudate nucleus) (Figure 1). ROIs were about 20-100 mm2 in size and were placed carefully to exclude the margins of the nucleis. All the statistics were assessed by SPSS 18.0 and Graphpad Prism 8.Results
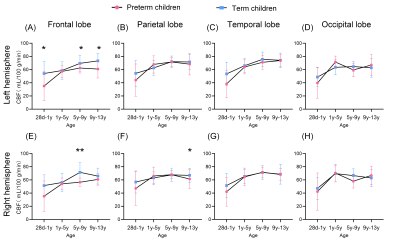
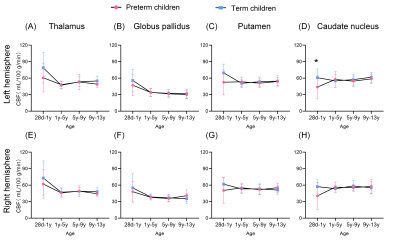
Of 129 children, 55 preterm (male/female, 29/26; GA range, 27~37weeks) and 75 term (male/female, 45/29; GA range, 37~42weeks) children were included (Table 1).Preterm children with postnatal age of 28 days to 1 year showed lower CBF than term children in left frontal lobe and left caudate nucleus (p<0.05) (Figure 2 and 3); while, no significant difference was observed in children with postnatal age range of 1 to 5year. For postnatal age range of 5 to 9 year, preterm children showed lower CBF than term children in left frontal lobe (p<0.05)(Figure 2), and CBF of right frontal lobe was significantly higher in term infants compared to preterm infants (p<0.01) ( Figure 2). For postnatal age range of 9 to 13 year, preterm children showed lower CBF than term children in left frontal lobe and right parietal lobe (p<0.05) (Figure 2).
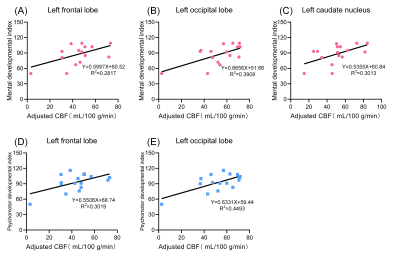
The mean MDI score for all 16 participants was 86.9 ± 19.0 (SD), and PDI score was 92.9±16.9 (SD). After controlling for age, MDI was positively correlated with CBF in the left frontal lobe (r=0.531, p=0.034), left occipital lobe (r=0.625, p=0.01) and left caudate nucleus (r=0.535,p=0.033). Meanwhile, positive correlations between CBF and PDI were found in the left frontal lobe (r=0.549, p=0.027) and left occipital lobe(r=0.670, p=0.004) when controlling for age (Figure 4).
Discussion
Main finding of our study was that preterm children showed lower CBF than term children in the frontal lobe, even at late childhood. Frontal lobe participates in advanced executive function, such as problem solving, planning, strategy development and implementation2. Previous study has demonstrated that the effects of preterm birth on intellectual development can extend even into early adulthood 3,4, a similar long lasting effect on cerebral perfusion was also observed in our results. We also found preterm children had lower CBF than term children in caudate nucleus, a part of basal ganglia whose function is motor planning and working memory decision-making. This may be another explanation to the effects of preterm birth on intellectual development. Meanwhile, positive correlations were observed between CBF and MDI, PDI in some regions, indicating higher CBF predicted better neurodevelopmental score.Conclusion
The effects of preterm birth on cerebral perfusion are long lasting and extend even into late childhood. Positive correlations between CBF and MDI, PDI are found in a number of regions in preterm infants.Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 81771810, 51706178, 81971581), National Key Research and Development Program of China (2016YFC0100300), the Clinical Research Award of the First Affiliated Hospital of Xi’an Jiaotong University (No. XJTU1AF-CRF-2020-005).References
1.Malamateniou C, Counsell SJ, Allsop JM,et al.The effect of preterm birth on neonatal cerebral vasculature studied with magnetic resonance angiography at 3 Tesla[J].Neuroimage.2006 Sep;32(3):1050–9.
2.Alfredo Ardila. On the evolutionary origins of executive functions[J].Brain Cogn.2008 Oct;68(1):92-9.
3.Taylor HG,Minich N,Bangert B,et al. Long-term neuropsychological outcomes of very low birth weight: associations with early risks for periventricular brain insults [J]. J Int Neuropsychol Soc.2004 Nov;10(7):987-1004.
4.Marlow N,Wolke D,Bracewell MA,et al. Neurologic and developmental disability at six years of age after extremely preterm birth[J].N Engl J Med,2005,352(1):9-19.
Figures