1629
Free-breathing T1-weighted black-blood vessel wall MRI based on radial imaging with motion sensitized driven equilibrium (MSDE) preparation1Philips Japan, Tokyo, Japan, 2Department of Radiological technology , Yuuai Medical Center, Okinawa, Japan, 3Department of Diagnostic and Interventional Radiology and Nuclear Medicine, University Hospital Hamburg-Eppendorf, Hamburg, Germany, 4Philips, Hamburg, Germany
Synopsis
Black-blood MRI is essential to characterize vessel wall in vivo and to identify vascular abnormalities. However, clear depiction of the wall structures in the thoracoabdominal region remains challenging and often suffers from pulsation or breathing artifacts. In this study, we employ motion sensitized driven equilibrium (MSDE) preparation technique and combine with radial-based 3D gradient- and 2D spin-echo imaging pulse sequences. Initial results in healthy volunteer and patients are reported in comparison to the conventional bright-blood and Cartesian techniques, which have shown promise in detection of vessel wall lesions before or after injection of contrast agent.
Introduction
Black-blood magnetic resonance imaging (MRI) is essential for diagnosis of vessel wall lesions and characterization of vascular abnormalities such as vasculitis or dissection 1. However, clear depiction of the vessel wall structures in the thoracoabdominal region remains challenging due to motions, where pulsation and breathing artifacts may introduce errors in measurement of wall characteristics 2. The previously described motion sensitized driven equilibrium (MSDE) preparation technique has shown promise in blood suppression independent from the inflow effect or blood T1 values, and can be used in conjunction with injection of paramagnetic contrast agents 3. The purpose of this work is to investigate technical feasibility of applying MSDE preparation in both gradient- and spin-echo pulse sequences based on radial sampling for free-breathing black-blood MRI before and after contract medium administration.Methods
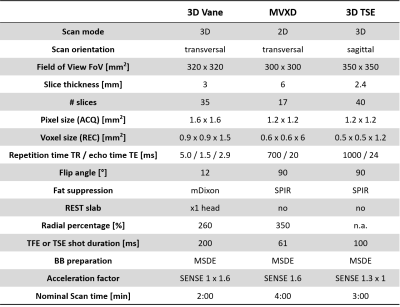
The improved MSDE (iMSDE) preparation scheme 4,5 was implemented to the following pulse sequences for free-breathing black-blood imaging: 1) 3D golden-angle radial stack-of-stars with dual-echo Dixon acquisition and semi-flexible echo times 6, indicated as 3D Vane-MSDE; 2) 2D multi-slice turbo spin echo (TSE) MultiVane XD (aka BLADE or PROPELLER) that employs rotating blades in the k-space for motion correction by matching low-resolution images reconstructed from each set of echo train segments 7, indicated as MVXD-MSDE. For iMSDE preparation, two 180° MLEV refocusing pulses were applied for inhomogeneity control 8,9 and additional bipolar gradients were inserted in the front for eddy currents compensation 9. All refocusing pulses were implemented as composite pulses (90x-180y-90x). Durations of the MSDE preparations were set to 14.5 ms shortest. Motion sensitized gradients were employed in the feet-head direction with velocity encoding set to 5 cm/s. The corresponding pulse sequence diagrams are shown in Figure 1. All human studies were performed on 3T whole-body clinical systems (Philips Ingenia, Best, the Netherlands). Additional respiratory motion correction via either navigator echo or camera 10 was applied in pre-contrast scans for comparison. In addition, conventional bright-blood 3D Vane without MSDE preparation, T2-weighted TSE MVXD, as well as Cartesian 3D TSE with respiratory triggering and black-blood MSDE preparation (3D TSE-MSDE) were included as reference. Typical imaging volume covered aortic arch for the thoracic part and aortic bifurcation including the common iliac arteries for the abdominal part. Basic imaging parameters were summarized in Table 1. For image analysis, the general image quality and artifacts was evaluated according to visual inspection. Moreover, vessel wall-to-blood contrast was assessed by quantitative measuring the contrast ratio (CR) based on the signal profile that was manually drawn across the vessel lumen.Results and Discussion
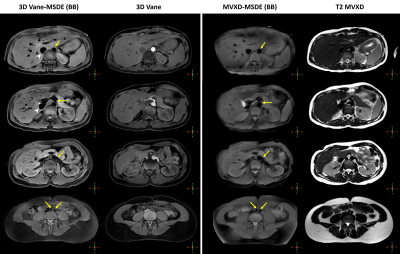
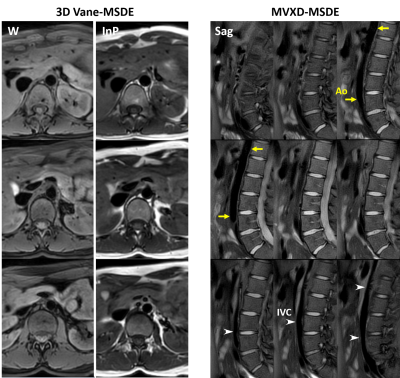
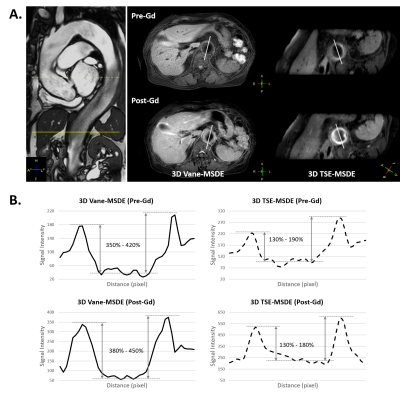
Four young healthy volunteers and two patients with clinically confirmed aortitis were included. Both techniques of 3D Vane and MVXD using MSDE preparation were able to provide homogeneous blood suppression inside the vessel lumen and delineate the vessel wall successfully in all imaging slices in the main thoracoabdominal vessels. These include both aorta and inferior vena cava, confirming that MSDE-based blood suppression is relatively independent of the inflow effect and flow velocities. The depicted vascular lumen was in good agreement to that in the conventional bright-blood 3D Vane without MSDE and T2 MVXD images. A typical example in a healthy volunteer was shown in Figure 2. Dual-echo Dixon acquisition in combination with free-breathing 3D Vane-MSDE provided additional in-phase images with non-fat-suppressed black-blood contrast (Figure 3), which may be of clinical relevance to observe pathophysiological changes in the practice. On the other hand, the obtained water images resulted in better fat suppression across the FOV compared to MVXD-MSDE with SPIR. Additional respiratory motion compensation using navigator echo was found to reduce motion-induced streaking artifacts that were typically seen in radial imaging, but was deemed not visually significant. In preliminary patient studies, quantitative analysis based on the signal profile across the lumen area revealed similar contrast ratio between the vessel wall and lumen before and after contrast administration. The analysis was performed in the selected images at both thoracic and abdominal levels (straight and dotted lines in Figure 4A), with one example shown in Figure 4B. This confirmed that MSDE preparation is relatively independent of the blood T1 values. Furthermore, good blood suppression was achieved in both 3D Vane-MSDE without respiratory motion correction and conventional Cartesian 3D TSE-MSDE with respiratory motion correction. However, the latter was found more subject to correction efficacy and image blurring shown with elevated the signal inside the lumen compared to the proposed method using 3D Vane-MSDE (Figure 4).Conclusion
Free-breathing black-blood vessel wall imaging is possible by combining MSDE preparation and radial imaging with gradient- or spin-echo pulse sequences in the thoracoabdominal area without additional respiratory compensation. Initial results in healthy volunteers and patients have shown promise in detection of vessel wall lesions associated with signal enhancement after injection of contrast agent. Further patient studies are needed to investigate its clinical performance.Acknowledgements
The authors thank PD Dr. Peter Bannas for helpful discussion of this work.References
1. Qiao Y, et al. Radiol (2014) 271:534.
2. Eikendal ALM, et al. J Cardiovasc Magn Reson (2016) 18:20.
3. Wang J, et al. Magn Reson Med (2007) 58:973.
4. Wang J, et al. J Magn Reson Imaging (2010) 31:1256.
5. Yoneyama M, et al. Magn Reso Med Sci. (2014) 13:277
6. Wuelbern JH, et al. Proc Int Soc Magn Reson Med (2015) 23:3648.
7. Pipe JG, et al. Magn Reson Med (2014) 72:430.
8. Wang J, et al. Proc Int Soc Magn Reson Med (2008) p.9616.
9. Obara M, et al. J Magn Reson Imaging (2014) 40:824.
10. Harder F, et al. Eur J Radiol (2019) 120:108675.
Figures