1617
3D time of flight MRA using radial-based gradient echo pulse sequence with modified DIXON of the aortic arch bifurcation1Philips Japan, Tokyo, Japan, 2Philips Healthcare, Best, Netherlands
Synopsis
Inflow magnetic resonance angiography (MRA) plays an important role in catheter insertion for intracranial endovascular treatment in the visualization of blood vessels at the aortic arch bifurcation. However, it is often difficult to accurately determine vascular stenosis due to respiratory artifacts and surrounding fat. In this study, we employ 3-dimensional time of flight MRA using radial-based gradient echo pulse sequence with modified DIXON (TOF-RADIXON) compared it with 3-dimensional time of flight MRA (TOF-MRA). The experimental results using TOF-RADIXON showed that ability to visualize blood vessels is more promising than TOF-MRA.
Introduction
In intracranial endovascular treatment, it is important to obtain morphological information of the blood vessel in order to advance the catheter to the target blood vessel. Recently, with the progress of non-contrast MRA, screening by the MRI has become widespread. In addition, 3-dimensional time of flight MRA (TOF-MRA) imaging1 is one of the most widely used techniques for easily assessing vascular morphology. However, depictions of the aortic bifurcations are often difficult to make an accurate diagnosis due to breathing artifacts and surrounding fat. Recently, various methods have been proposed, for example cardiac-gated 3D Fast-spin-echo non-contrast-enhanced-MRA2 and REACT3, but they are sensitive to motion. Radial sampling4 is promising for suppressing breathing artifacts and can be combined with modified DIXON (mDIXON)5 for water and fat separation. The purpose of this work is to investigate the technical feasibility of applying 3-dimensional time of flight MRA using radial-based gradient echo pulse sequence with mDIXON (TOF-RADIXON) for accurate vascular morphology evaluation.Methods
Experiments: A total of 3 volunteers were examined on a 1.5T whole-body clinical system (Ambition, Philips Healthcare). The study was approved by the local IRB, and written informed consent was obtained from all subjects.None-contrast-enhanced TOF images of the aortic bifurcations acquired as using the TOF-RADIXON and TOF-MRA. The TOF-RADIXON and TOF-MRA images were finally visualized by computing maximum intensity projection images (MIP). MIP created images with the background left and images with the background cut out.
TOF-RADIXON: The TOF-RADIXON sequence was acquired with FOV=250mm, acquisition voxel size=1.2*1.2*2.0(-1.0)mm3, TE(1st,2nd)/TR=1.98,3.7/10ms, FA=10, water and fat separation technique =mDIXON, 100 slices, single volume and scan duration=1m46s.
TOF-MRA: The TOF-MRA sequence was acquired with FOV=250mm, acquisition voxel size=0.7*1.2*2.0(-1.0)mm3, TE/TR=6.9/16ms, FA=17(13-17-21), SENSE=1.5, 100 slices, single volume and scan duration=1m34s.
Evaluation: The image quality of the TOF-RADIXON and the TOF-MRA was compared between the original image and MIP with/without background. Image quality was evaluated by observers (a radiologist and two radiographer) in consensus on a four-point scale regarding sharpness, presence of breathing artifacts at the levels of measurement, and anatomic delineation. Quality was rated on a Likert scale of 1 to 4: 1 non-diagnostic, 2 poor image quality with substantial blurring impairing diagnostic confidence, 3 intermediate image quality with mild blurring, and 4 good image quality without any blurring and resulting high diagnostic confidence.
Results and Discussions:
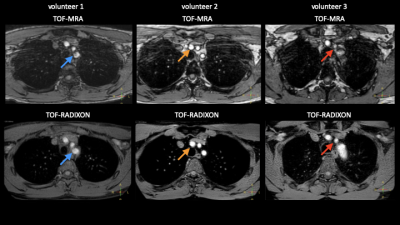
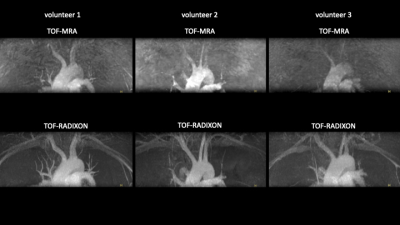
Figure 1 is the source images of the TOF-RADIXON and the TOF-MRA. In the TOF-RADIXON, images were obtained without signal deficiency in the vascular lumen (blue arrow), overlap of fat movement artifacts due to breathing with vascular signals (orange arrow), and signal deficiency in the blood vessels due to breathing (red arrow). Figure 2 is a MIP images with a background. The images with the background left was MIP image in the TOF-RADIXON, in which the high signal of fat was uniformly suppressed and the blood vessel visualization ability was excellent. Figure 3 is images of the background cut by post-processing. In the TOF-RADIXON, the bifurcation of the blood vessel branching from the aortic arch had high visualization ability without blurring or overlapping of fat. The TOF-RADIXON scored higher than the TOF-MRA in all results of Likert scale.Therefore, it was suggested that the TOF-RADIXON has high vascular imaging ability due to the reduction of mmotion artifact by radial sampling and the robust separation of water and fat using mDIXON.Conclusion:
The TOF-RADIXON demonstrated high blood vessel visualization using mDIXON without additional motion compensation.Acknowledgements
No acknowledgement found.References
1 Parker DL, Yuan C, Blatter DD. MR angiography by multiple thin slab 3D acquisition. Magn Reson Med 1991; 17: 434– 451.
2 Miyazaki M, Sugiura S, Tateishi F, Wada H, Kassai Y, Abe H. Non‐contrast‐enhanced MR angiography using 3D ECG‐synchronized half‐Fourier fast spin echo. J Magn Reson Imaging 2000; 12: 776– 783.
3 Yoneyama M, Zhang S, Hu HH, Chong LR, Bardo D, Miller JH, et al. Free-breathing non-contrast-enhanced flow-independent MR angiography using magnetization-prepared 3D non-balanced dual-echo Dixon method: a feasibility study at 3 tesla. Magn Reson Imaging. 2019;63:137–46.
4 Lauterbur P.C. Image formation by induced local interactions: Examples employing nuclear magnetic resonance. Nature. 1973;242:190-191.
5 Eggers H, Brendel B, Duijndam A, Herigault G (2011) Dual-echo Dixon imaging with flexible choice of echo times. Magn Reson Med 65:96–107
Figures