1611
Feasibility of Free-Breathing Non-contrast Magnetic Resonance Pulmonary Angiography1Peking University First Hospital, Beijing, China, 2MR Collaboration, Siemens Healthcare Ltd, Beijing, China, 3MR APP, Siemens Healthcare Ltd, Beijing, China
Synopsis
We investigated the feasibility and clinical value of free-breathing non-contrast MR pulmonary angiography (MRPA). The subjective diagnostic image quality values, evaluated by two radiologists, showed excellent consistency. Non-contrast MRPA can provide acceptable image quality that can be applied broadly in clinical medicine.
Introduction
CT pulmonary angiography (CTPA) is currently considered the imaging standard of care for the diagnosis of pulmonary embolism (PE). However, CTPA has important drawbacks in that it requires ionizing radiation, which is especially troublesome when imaging young and pregnant patients. It also uses iodinated contrast material that carries the risk of nephrotoxicity and occasional severe allergic reactions. Recent advances in magnetic resonance pulmonary angiography (MRPA) techniques have led to the increased use of this modality for the detection of PE in proper clinical settings since MRPA does not require either iodinated contrast or ionizing radiation1-4.This study aimed to investigate the feasibility and clinical value of non-contrast MRPA.Methods
This study consisted of 29 healthy volunteers (13 males, mean age: 44.1 ± 8.0 years) who were given written informed consent. All non-contrast MRPA data were collected on a 1.5T MR scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) with an 18-channel body coil and an integrated 32-channel spine matrix coil. A free-breathing 3D turbo spin-echo (TSE) with variable-flip-angle sequence (SPACE) was used to acquire non-contrast MRPA data with the following parameters: TR=2200 ms, TE=102 ms, TI=180ms, field of view (FOV)=380×285 mm2, slices per slab=56, slice thickness=4 mm, matrix size=320×230, voxel size=1.2×1.2×4 mm3, flow compensation in the readout direction, and acquisition time=3 min 54 s. The subjective image quality assessment of normal pulmonary arteries was evaluated by two experienced radiologists. The total image quality was evaluated on a 5-point scale for a clear demonstration of pulmonary branches: 5 – sixth pulmonary branches, 4 – fifth pulmonary branches, 3 – fourth (subsegmental) pulmonary branches, 2 – third (segmental) pulmonary branches, and 1 – main, left, and right pulmonary artery trunk and lobular pulmonary branches. Images with a score ≥ 3 were considered satisfactory. Image quality of the main, left, and right pulmonary arterial trunk was separately evaluated on a 4-point scale: 4 – vessel was sharply defined, and there were no artifacts, 3 – minor blurring, 2 – adequate diagnostic image quality with mild blurring, and 1 – nondiagnostic. Image quality inter-observer agreement was assessed by the Kappa test.Results
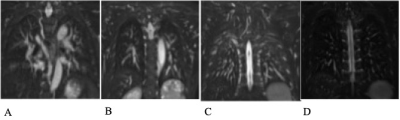
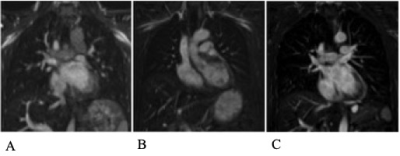
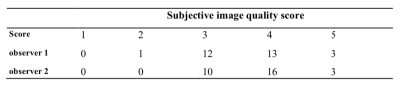
All subjects in the study group completed the examination successfully. Example images and their respective scores are displayed in Figure 1 (branch image quality) and Figure 2 (pulmonary artery trunk image quality). The main trunk and proximal branch of the pulmonary artery were demonstrated clearly on the MRPA images. A summary of the subjective image quality scores from the two observers is presented in Table 1. Only one case was assigned a score of 2. Satisfactory scores (≥3) were given to 96.6% (observer 1) and 100% (observer 2) of the total images, with a mean total image quality score of 3.6 ± 0.7(observer 1) and 3.8± 0.6(observer 2). The kappa value was 0.77 for total image quality between two the observers. The mean image quality scores of the main, left, and right pulmonary arterial trunks were 3.1 ± 0.5, 3.0 ± 0.6, 3.2 ± 0.6 (observer 1) and 3.1 ± 0.5, 3.1 ± 0.5, 3.2 ± 0.7 (observer 2). Image quality kappa values for these vessels were 0.84, 0.79, and 0.70, respectively. The subjective diagnostic quality values evaluated by the two radiologists showed excellent consistency. Any disagreement in the image quality scores between the two reviewers was limited to a score difference of 1.Discussion and conclusion
MRPA is an important alternative to CTPA in younger patients where the effects of ionizing radiation are of concern. MRPA is also beneficial in patients with allergies to iodinated contrast and patients at risk of contrast-induced nephropathy. Novel non-contrast MRPA techniques are increasingly available and could prove beneficial in evaluating PE in pregnant patients. Patients who are severely dyspneic might be unable to perform adequate breath-holds, making it easy to perform non-contrast MRPA, which does not require breath-holding1, 2.In conclusion, non-contrast MRPA can provide acceptable image quality and could be applied broadly in clinical medicine.
Acknowledgements
No acknowledgement found.References
1. Muhammad A, Mayil K, Ananth JM, et al. Update on MR imaging of the pulmonary vasculature. Int J Cardiovasc Imaging 2019; 35 (8): 1483-1497
2. Prabhakar R, Michael AB. Cardiovascular MR Imaging at 3T: Opportunities, Challenges, and Solutions. Radiographics 2014; 34:1612–1635
3. Donald GB, Mark LS, Michael DR, et al. Contrast-enhanced pulmonary MRA for the primary diagnosis of pulmonary embolism: current state of the art and future directions. Br J Radiol 2017; 90 (1074): 20160901
4. Scott KN, Mark LS, Michael DR. Contrast Enhanced Pulmonary Magnetic Resonance Angiography for Pulmonary Embolism: Building a Successful Program. Eur J Radiol 2016; 85 (3): 553–563
Figures